12 Brain and Cranial Nerves Lab
"We are all now connected by the internet, like neurons in a giant brain." - Stephen Hawking
Gillian Backus; Heidi W. Wangerin; and Paula Rodgers
Objectives
The Brain:
- Identify and describe the function(s) of parts of the brain on both an image and model.
- Identify the starred (*) structures from the terminology checklist on a sheep’s brain.
- Identify the meninges and the spaces created by the meninges on both an image of the brain and on a brain model.
- Trace the flow of cerebrospinal fluid (CSF) through the brain from its origin in the choroid plexus to where it collects in the superior sagittal sinus.
- Given the location of a brain lesion of a specific part of the brain, predict the effect the lesion will have on brain function.
The Cranial Nerves:
- Identify and describe the basic function(s) of the 12 cranial nerves on an image or model.
- Categorize each cranial nerve as sensory, motor, or both (mixed).
- Evaluate cranial nerve function from the results of common cranial nerve tests.
Terminology Checklist
Structures marked with * must also be identified on the sheep brain.
Regions of the Brain
|
Functional Areas of the Cerebrum
|
Other Structures of the Brain
|
Flow of Cerebrospinal Fluid
|
Cranial Nerves
|
Outline
Case Study: “Stumbling Stan”
Activity 1: The Structure and Function of the Brain
Activity 2: The Meninges and the Flow of Cerebrospinal Fluid
Activity 3: Dissection of the Mammalian Brain (Sheep)
Activity 4: Identify the Cranial Nerves
Activity 5: Evaluation of Cranial Nerve Function
Putting It All Together
Case Study: “Stumbling Stan”
It’s a busy night in the city’s emergency department (ER). Paramedics bring in a 20- year-old man named Stan by ambulance. He is writhing in pain due to a terrible headache, can’t answer questions properly (he doesn’t know today’s date), doesn’t understand where he is, and is experiencing sudden loss of vision. As the paramedics move him into a hospital bed, he reels and vomits. He is conscious but confused. His speech is slurred. The physician orders an MRI of his head to evaluate the brain and surrounding structures, and a cranial nerve exam.
From the case study above, describe the symptoms of the patient.
Activity 1: The Structure and Function of the Brain
Materials:
- brain model
- terminology labels with sticky tack
Background:
Magnetic resonance imaging (MRI) uses a powerful magnet that can create detailed cross-sectional images of bone and soft tissue. An MRI is ordered to image the patient’s brain to look for structural damage. In this activity, you will explore the anatomical features of brain including the main regions and their functions using a brain model.
For convenience, anatomists divide the brain into four main regions: the cerebrum (the “foldy” part of the brain), the cerebellum (the “smaller brain” at the posterior surface), the brainstem (superior to the spinal cord) and the diencephalon (the distinct interior parts of the brain, as seen in sagittal section).
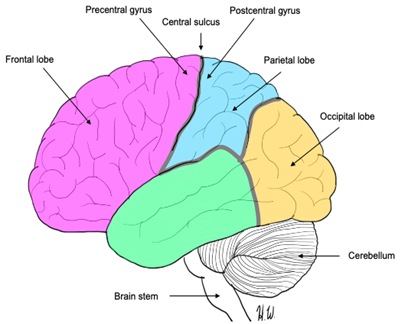
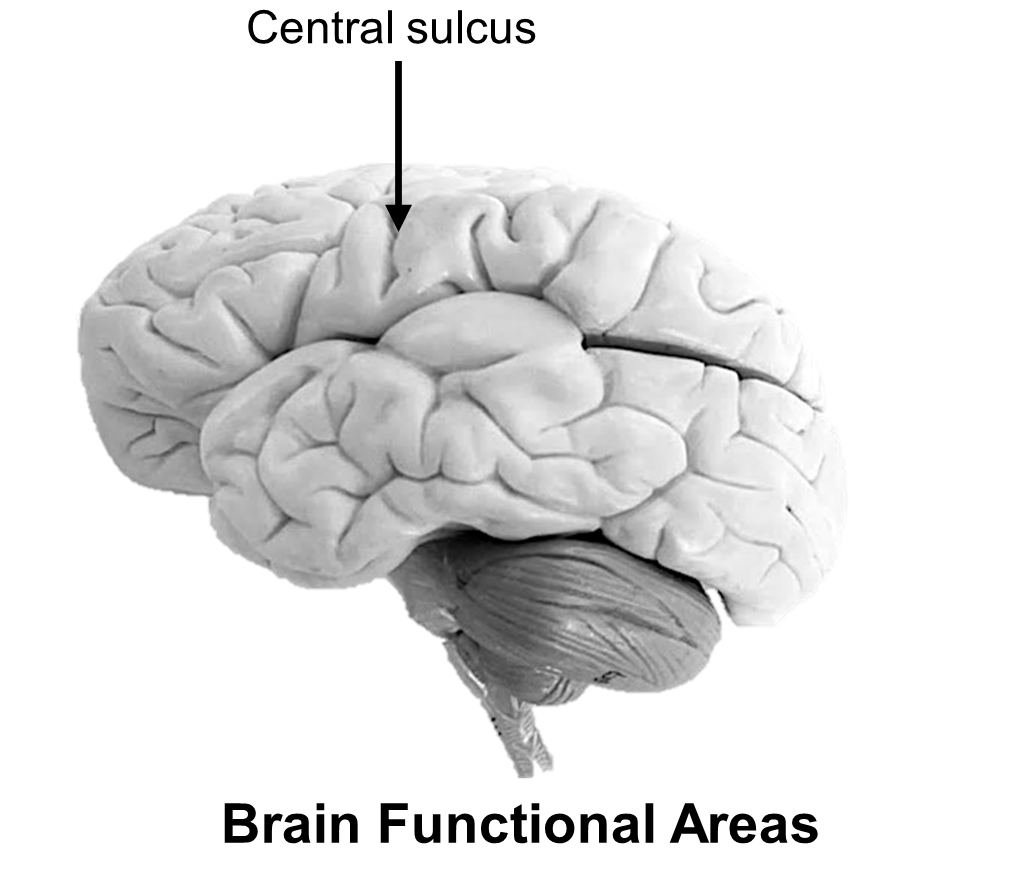
Figure 1: Lobes of the cerebrum (insula not shown on image as it is deep to the temporal lobe).
Organization of the cerebrum (Figures 1 and 2)
The largest part of the brain, the cerebrum, is characterized by bumps called gyri and the depressions between them, called sulci. There are also deeper, groove-like fissures. Both fissures and sulci serve as landmarks to divide the cerebrum into specific regions. The longitudinal fissure runs midsagittally and divides the cerebrum into equal right and left halves called hemispheres. The frontal lobe is the most anterior and is deep to the frontal bone of the skull. The left and right parietal lobes are posterior to the frontal lobe and are located directly under the parietal bones. The left and right temporal lobes are deep to the temporal bones, near the ear, and the occipital lobe is at the posterior of the skull, under the occipital bone (Figure 1). The lateral fissure (sulcus) is a deep groove that runs transversely and separates the frontal and parietal lobes from the inferior temporal lobe. The fifth lobe, the insula, is found deep to the lateral fissure.
Diencephalon (Figure 2)
The diencephalon is located deep to the cerebrum where you will find three specific subparts of the brain: the thalamus, which serves as a major relay station for the signals entering the brain, the hypothalamus, a major neuro-endocrine center that controls many homeostatic mechanisms including temperature, heart rate, and respiratory rate, and the epithalamus (Figure 2). The epithalamus contains the pineal gland, a melatonin-secreting gland responsible for controlling circadian rhythms and sleep-wake cycles. The pituitary gland, while not strictly part of the diencephalon, hangs from a short, narrow stalk inferior to the hypothalamus, called the infundibulum.
Brainstem (Figures 2 and 3)
Evolutionarily the oldest part of the brain, this region is the swelling at the base of the spinal cord. The brain stem holds many autonomic and survival functions critical for life. This part of the brain is instinctual. It has three main subparts: the most inferior part of the brainstem is called the medulla oblongata and is responsible for controlling critical reflexes for breathing and heart rate. Just above the medulla oblongata is a larger swelling called the pons. This structure serves as a bridge between the medulla and the midbrain. The pons contains centers for sleep-wake cycles (Figure 2). The midbrain is the most superior part of the brainstem and is itself made of subparts. The superior and inferior colliculi are visible on the posterior surface of the brainstem when the cerebrum and cerebellum are wedged apart. The two superior and two inferior colliculi make four small bumps that are collectively called the corpora quadrigemina (Figure 2). These structures are responsible for visual and auditory reflexes, respectively.
Figure 2: Midsagittal view of the brain showing structures of the diencephalon, midbrain, and cerebellum. Structures with a * make up the brainstem.
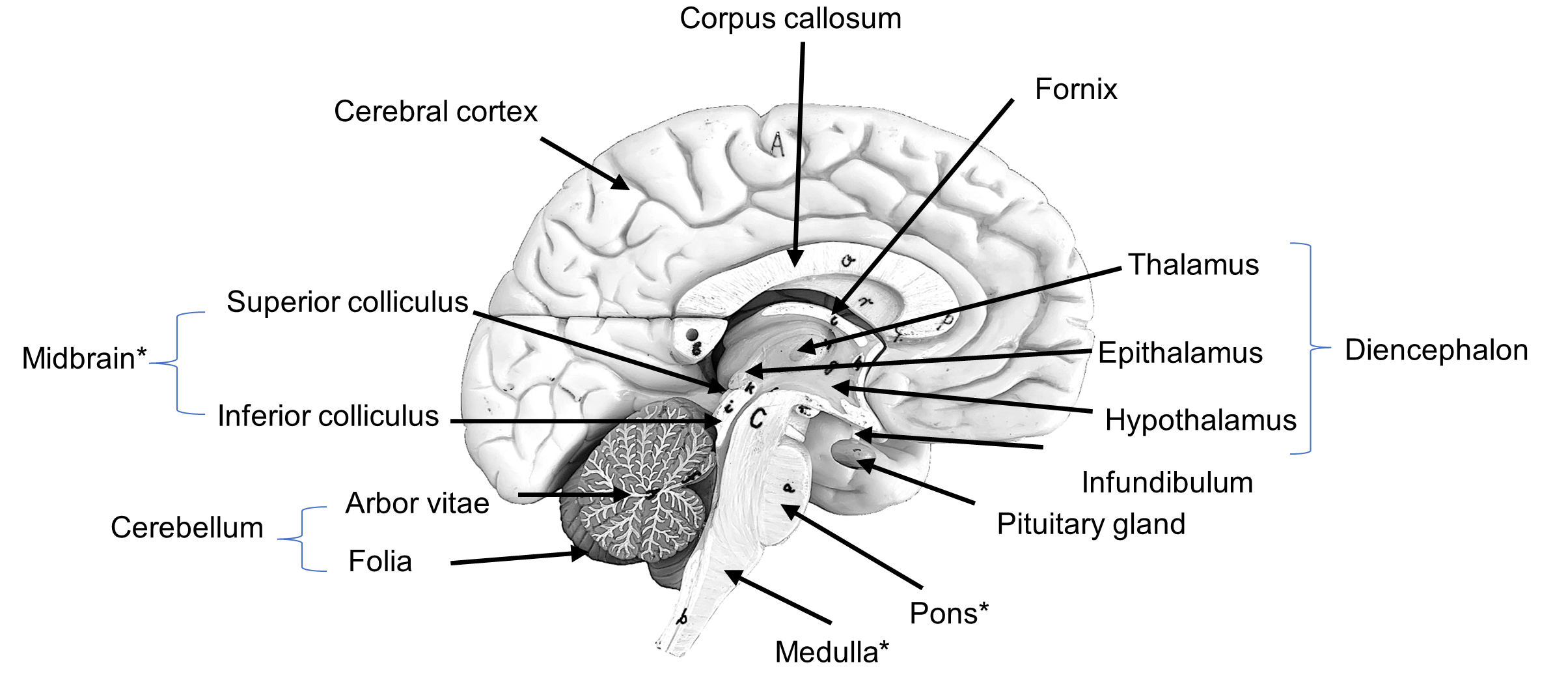
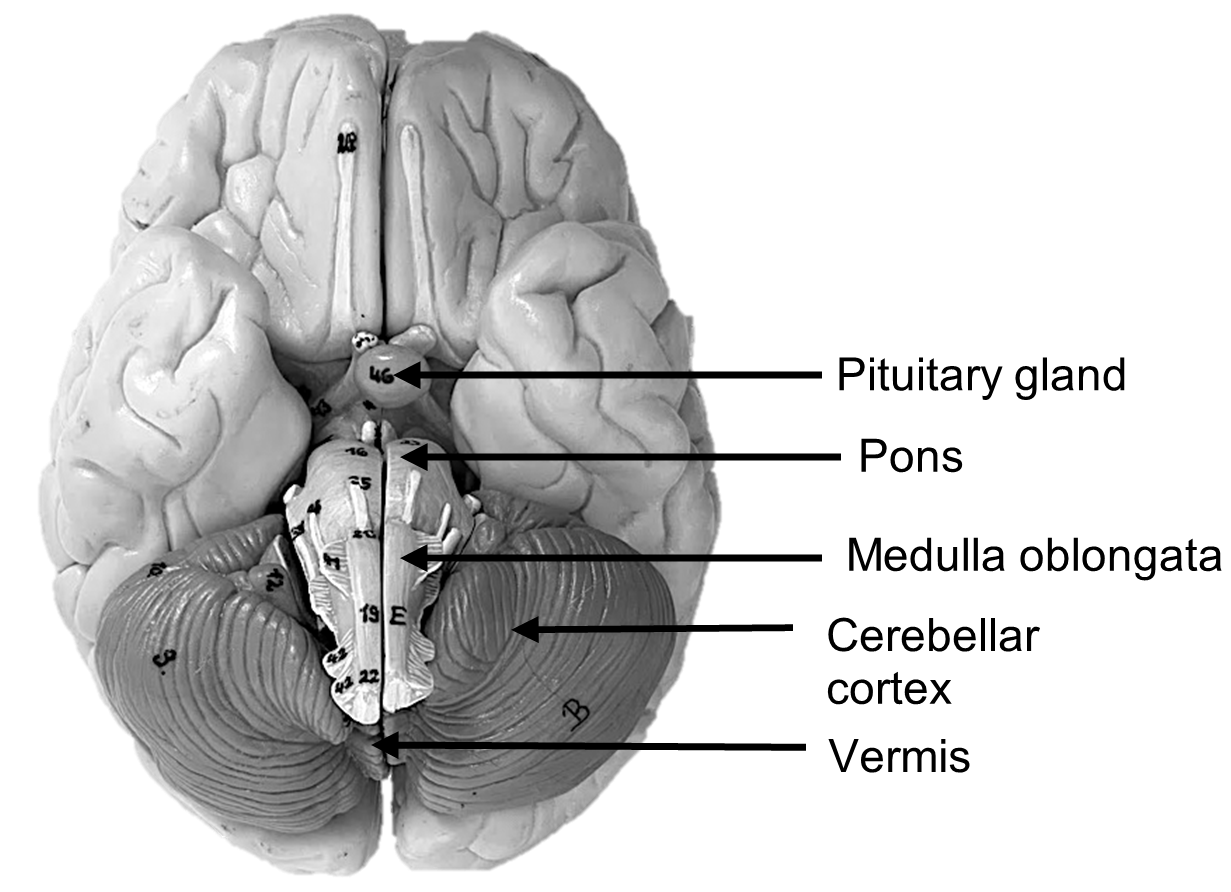
Cerebellum (Figures 2 and 3)
The cerebellum is a small lobular structure tucked inferiorly to the occipital lobe at the posterior surface of the brain. It is composed of an outer gray matter called the cerebellar cortex which contains folds, folia, that are smaller than the gyri of the cerebrum (Figure 2). The cerebellum, like the cerebrum, has two hemispheres divided at the midpoint by a structure called the vermis, a worm-like structure (Figure 3). When cut in sagittal section, a tree-like network of myelinated axons called the arbor vitae (tree of life) can be seen (Figure 2). The function of the cerebellum is to maintain balance and to coordinate skeletal muscle contractions to ensure smooth movement. The cerebellum constantly monitors proprioception, and thus allows you to stand on one foot with your eyes closed and touch your nose at the same time.
Figure 3: Inferior view of brain.
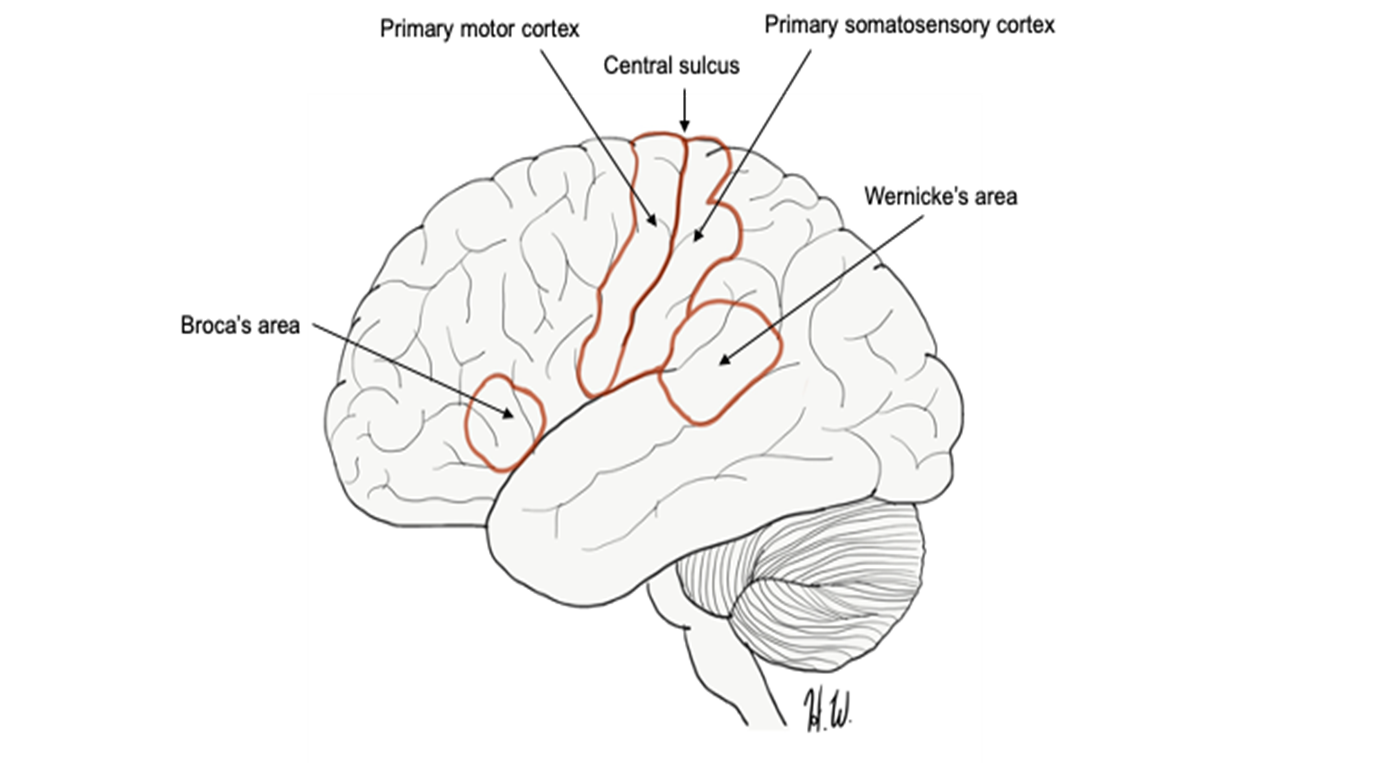
Functional regions of the cerebral cortex (Figure 4)
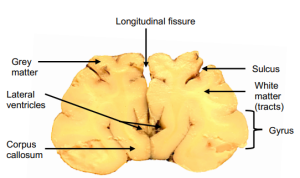
The cerebrum is responsible for many higher mental functions such as learning, memory, and language and is considered the “thinking brain”. The cerebral cortex is mostly gray matter composed mainly of the nuclei of the neurons while the white matter is composed of myelinated axons, or tracts. Two prominent tracts of white matter in the cerebrum are the corpus callosum and the fornix (Figure 2). The corpus callosum connects the right and left halves of the cerebrum, and the fornix connects the cerebrum to lower regions of the brain. The lobes of the cerebrum have many specific functional areas within them. For example, the primary somatosensory cortex which is located just posterior to the central sulcus in an area called the postcentral gyrus, is responsible for perceiving and coordinating senses like temperature, touch, vibrations, stretch, and position of the joints. The primary motor cortex is located anterior to the central sulcus, in the precentral gyrus. The primary motor cortex is responsible for planning and executing movement. Other important functional areas of the cerebrum include the Broca’s area, located just anterior to the temporal lobe, in the frontal lobe, and Wernicke’s areas, located just superior to the temporal lobe, in the parietal lobe (Figure 4). Both small areas control aspects of speech. Broca’s area controls the formation of speech (motor movements) while Wernicke’s area is responsible for comprehension of language.
Figure 4: Functional areas of the cerebrum (lateral view).
Procedure:
1. Using the brain model, background information, and the sticky labels, label the parts of the brain model.
2. Once you have labelled all the structures on the brain model, ask your instructor to check the model and initial below.
Instructor’s Initials for labeled brain model: _____________
3. Use the terms provided to color in the functional regions of the cerebrum on the image below: primary somatosensory cortex (blue), primary motor cortex (red), Broca’s area (orange), and Wernicke’s area (black).
4. QUIZ TIME! Your instructor will provide you either with notecards with which to identify structures or will set up a quiz on the back bench for you to test yourself.
Instructor initials here for completed quiz: ___________
5. Your patient Stan has trouble producing speech. Circle the part(s) on the figure you colored above that are probably involved in his inability to form words.
Activity 2: The Meninges and the Flow of Cerebrospinal Fluid
Materials:
- CSF sagittal section model
- sticky terminology labels
- ventricle model
Background:
Stan’s MRI indicates that there is enlargement of the ventricles, spaces filled with cerebrospinal fluid. A blockage in the flow of this fluid or a bacterial infection are common causes of these findings. In this activity you will explore the location and movement of cerebrospinal fluid (CSF) in and around the brain.
Meninges are protective coverings surrounding the brain and spinal cord. The meninges are made of connective tissue. There are three different meninges, piled on top of each other; they wrap the brain like a carefully packed shipping box. The outermost layer, the dura mater, is durable and tough like a cardboard box. It is made of dense irregular connective tissue. The middle layer, the arachnoid layer, has a spidery, netlike appearance, and is similar in function to bubble wrap. The innermost layer, the pia mater, is the thinnest layer like tissue paper. It adheres to the brain so tightly that it cannot be separated from it.
In between each meningeal layer is a space (or potential space). Above the dura mater is the epidural space which is filled primarily with adipose tissue. The subdural space is under the dura mater (this is a potential space), and the subarachnoid space is under the arachnoid layer (Figure 5).
Figure 5: Close-up of sagittal sinus arachnoid granulation.
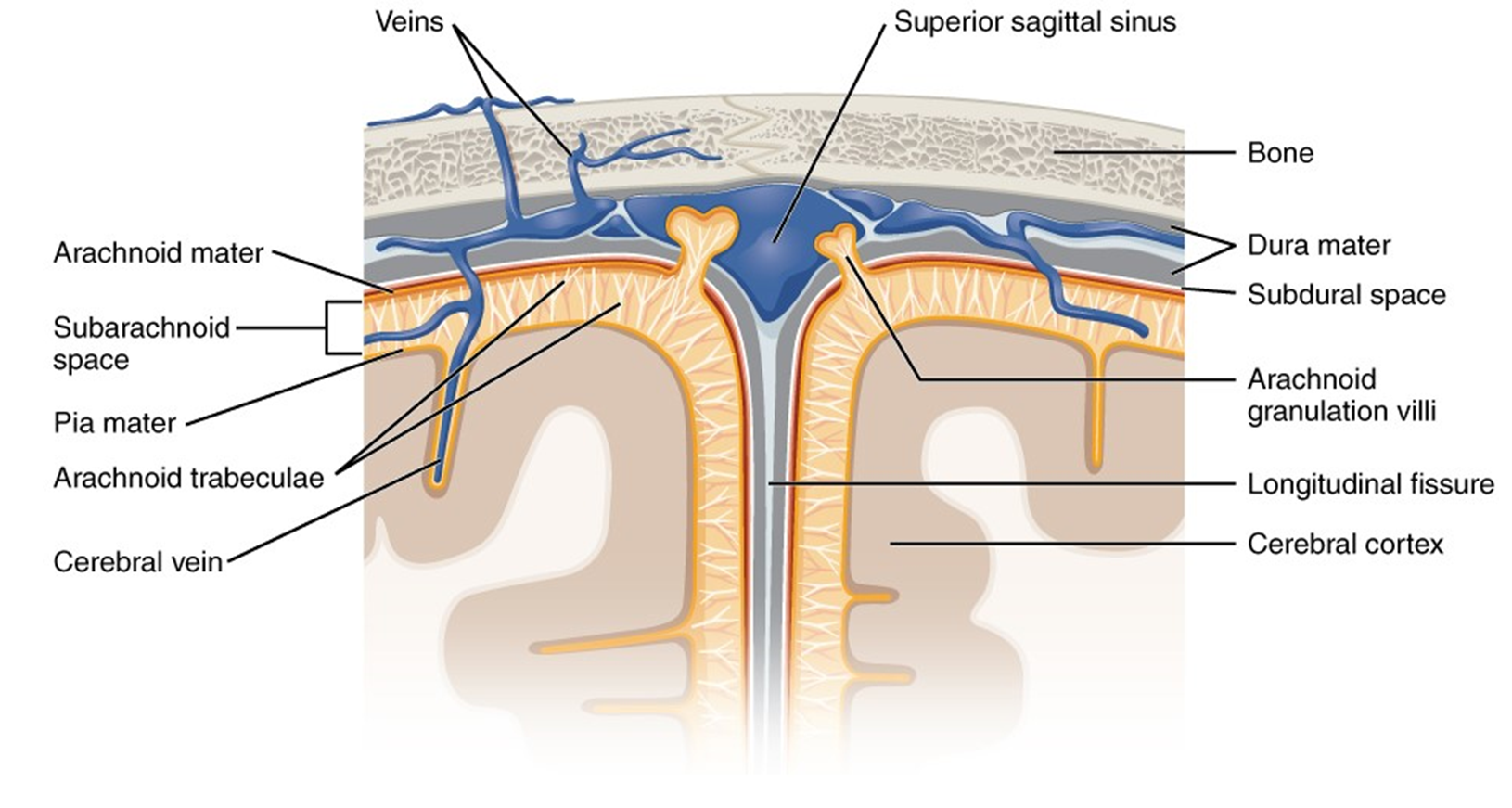
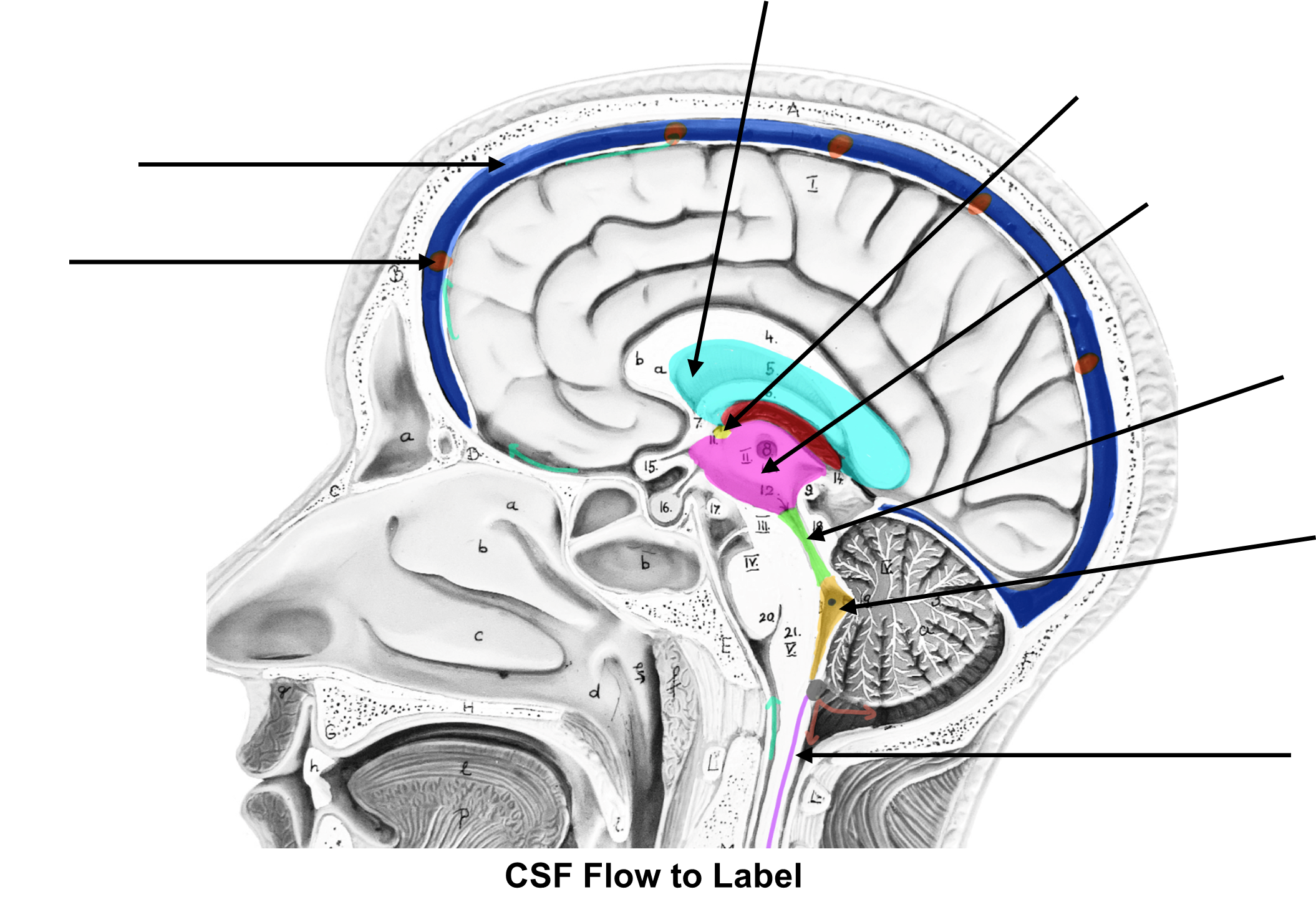
Circulating within the subarachnoid space is a special nutrient-rich but acellular fluid called cerebrospinal fluid (CSF). This fluid is formed from a selective filtration barrier lined with ependymal cells called the choroid plexus. On one side, the choroid plexus contains a tuft of capillaries. Nutrients diffuse out of the blood and are filtered by the ependymal cells to form clear CSF. All brain and spinal cord nervous tissues are bathed by this special fluid. This is how the nervous tissue receives nutrients and removes cellular wastes even though the brain itself contains no blood vessels and no blood.
The circulation of the CSF throughout the brain and spinal cord is important to understand. After it is formed at the choroid plexus, the CSF collects in the lateral ventricles. As it accumulates, it passes through the interventricular foramina into the third ventricle, a centrally located ventricle between and slightly inferior to the lateral ventricles. CSF then drains into the cerebral aqueduct to the fourth ventricle, located at the boundary of the cerebellum and brain stem. From here, CSF empties into the subarachnoid space via tiny holes called apertures, and into the central canal of the spinal cord. The subarachnoid space surrounds the brain and spinal cord and the central canal is centrally located in the middle of the spinal cord itself. Thus, the entire brain and spinal cord are cushioned with CSF from the inside and out. For a flow chart, see the textbox below.
Choroid plexus of lateral ventricles → interventricular foramen → third ventricle → cerebral aqueduct → fourth ventricle → subarachnoid space via (apertures) and central canal → arachnoid granulations → superior sagittal sinus → venous circulation
Figure 6: Midsagittal section of the head, showing circulation or cerebrospinal fluid (CSF), black arrows.
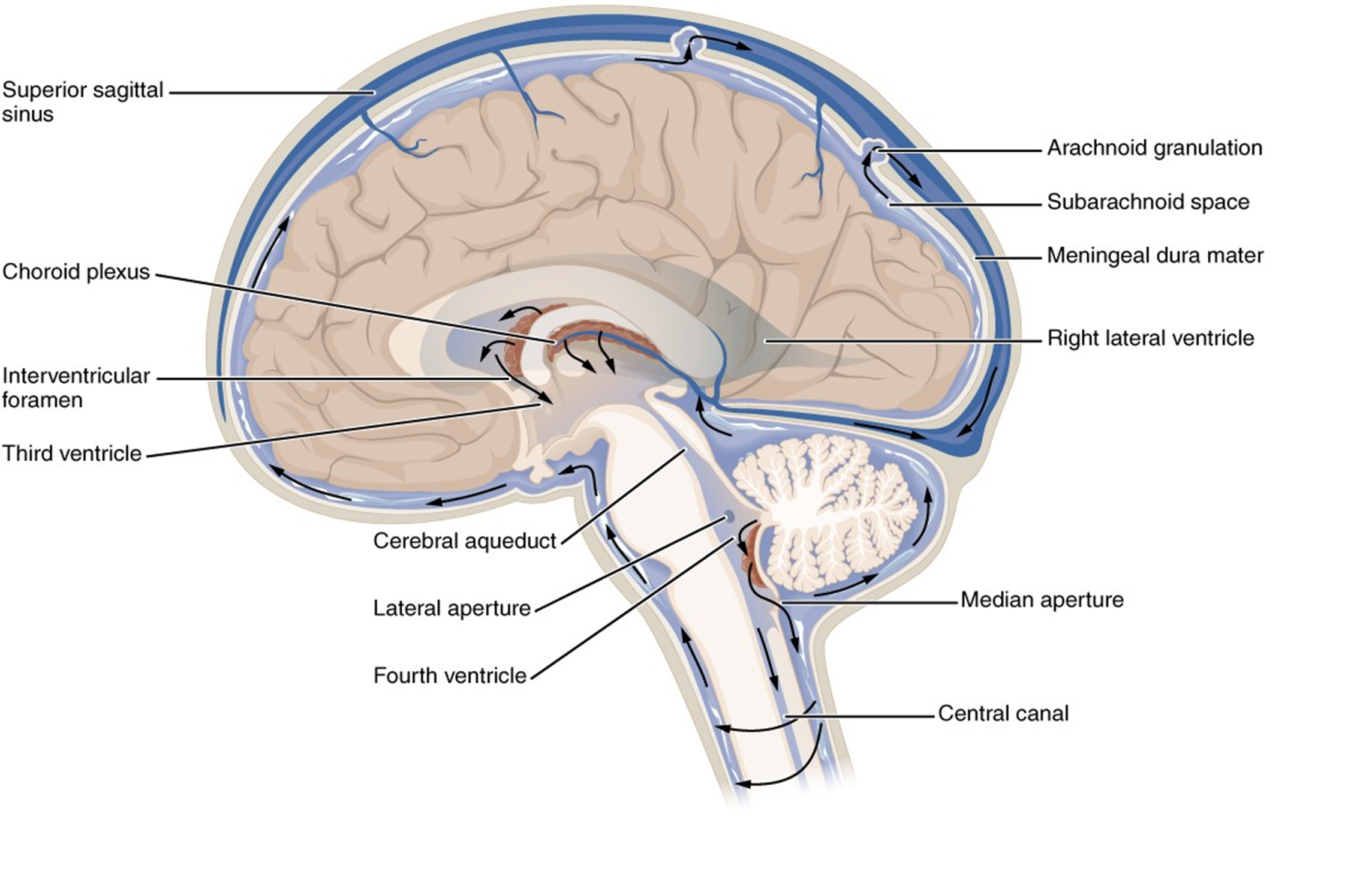
Cerebrospinal fluid is constantly renewed and recycled, by way of out-pockets of the arachnoid mater called the arachnoid granulations. The arachnoid granulations, part of the arachnoid mater, protrude through the dura mater and into the superior sagittal sinus (Figure 6). This is where the cerebrospinal fluid returns to the venous circulation and ultimately, to the heart.
Stan received a spinal tap (or lumbar puncture) to help diagnose his problem. Doctors removed 20 ml of CSF from the subarachnoid space using a needle inserted between lumbar vertebrae 3 and 4 (L3 and L4). The CSF was found to cloudy and has presence of elevated white blood cells and bacteria indicate bacterial infection in the brain, a common cause of meningitis. These findings, combined with his symptoms, are consistent with a diagnosis of hydrocephalus (“water on the brain”) due to bacterial meningitis. Inflammation of the meninges impedes the flow of CSF; the fluid has built up around his brain, putting pressure on the delicate brain tissue. Stan needs immediate surgery to create a shunt to remove the excess fluid. He will also receive a heavy course of antibiotics to treat bacterial meningitis.
Procedure:
1. On a model of ventricles use the terminology labels to identify the structures. Label the diagram below with the labels pertaining to CSF formation and circulation (arachnoid granulation, superior sagittal sinus, lateral ventricle, interventricular foramen, third ventricle, cerebral aqueduct, fourth ventricle, central canal).
Activity 3: Dissection of the Mammalian Brain (Sheep)
Materials:
- disposable gloves
- dissecting tray and foam pad
- dissection tools (blunt probe, scalpel, fine probe, scissors)
- lab apron
- safety goggles
- sheep brain
Background:
In this experiment, you will compare a sheep brain to the human brain, paying close attention to the similarities and differences in structure. Humans stand upright, while sheep stand on all fours. Thus, please note that the orientation of the brain to spinal cord is different from that of a human brain as the spinal cord emerges from the posterior surface of the brain, rather than from the inferior surface, as in humans. In addition, sheep, like most mammals, have an acute sense of smell — much better than ours. Thus, you will easily be able to identify the large swellings on the inferior surface of the brain at the anterior end. These are the olfactory bulbs. They are larger in sheep than in human brains. In many ways, though, the sheep brain is quite similar to our own. It has the same four basic regions and many of the same parts.
Procedure:
**You must wear lab gloves, a lab apron and safety goggles for this dissection.
1. Collect a dissecting tray, and dissecting tools. Grab a few paper towels for clean-up.
2. Remove a specimen from the bucket using the slotted spoon.
3. Find three of the four main brain regions: cerebrum, cerebellum, and brain stem (Figure 7). These are visible from an external view.
4. Turn the brain to its dorsal surface (back view) to observe the longitudinal fissure (Figure 8).
5. On the posterior side of the brain, with a thumb and forefinger or gently using a probe, separate the cerebrum and the cerebellum gently apart from each other to reveal a series of four bumps (Figure 9). This is the corpora quadrigemina, a four-part structure made of two superior colliculi and two inferior colliculi. The two superior colliculi play a role in visual reflexes, while the inferior colliculi are responsible for auditory reflexes.
6. Turn the brain to observe the ventral surface. Find the large olfactory bulbs, and the optic chiasma (Figure 10). The optic chiasma has an “X” shape and is made of white matter. The two anterior parts of the “X” are parts of the optic nerve that bring visual input to the brain from the eye and the two posterior sides of the “X” are called optic tracts. The optic tracts lead to the occipital lobe for visual processing.
7. You may also be able to see the pituitary gland attached by a tiny stalk called the infundibulum. On your specimen, this structure may have gotten torn off, as it is delicate and only thinly held to the underside of the brain.
8. Now you are ready to make a midsagittal section along the longitudinal fissure (this may already have been done for you) of the brain to separate it into 2 halves. Find each of the remaining starred structures from your terminology sheet.
9. Your instructor will show you a frontal section (Figure 11). Note the longitudinal fissure. You can distinctly identify the white matter (tracts) from the grey matter. A section of white matter runs just inferiorly to the longitudinal fissure, called the corpus callosum. In this view the lateral ventricles are also visible.
10. Look closely at the sheep brain to determine how it is different to a human brain. Name at least two ways that the sheep brain differs from the human brain:
Figure 7: External view of sheep brain.
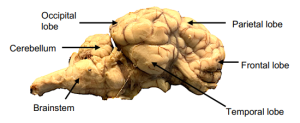
Figure 8: Sheep brain dissection, dorsal view.
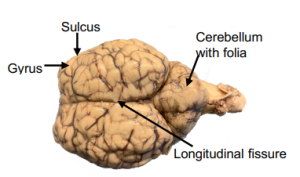
Figure 9: Posterior of sheep brain illustrating corpora quadrigemina.

Figure 10: Ventral view of sheep brain.
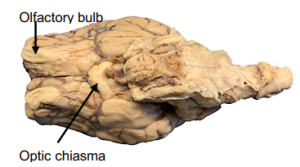
Figure 11: Frontal Section of sheep brain.
11. QUIZ TIME! Take 10-15 minutes to study the sheep brain with your lab partner. Study both external and internal anatomical terms. Once you have mastered the structures of the sheep brain, ask your instructor to quiz you on 5 structures and then have the instructor initial here.
Instructor initials here for completed quiz: ___________
12. To cleanup, place the sheep brain back in the dissection bucket.
13. Thoroughly clean your dissecting tools with soap and water. Dry them with paper towels and once dry, put them away.
14. Remove the blue dissecting pad from the dissecting tray and rinse the dissecting pad and place it on the drying rack. Please rinse and tray the dissecting tray and leave them unstacked by the sink.
15. Wipe down your lab bench with disinfectant.
Activity 4: Identify the Cranial Nerves
Materials:
- brain model
- colored pencils
- laminated terminology labels and sticky tack
Background:
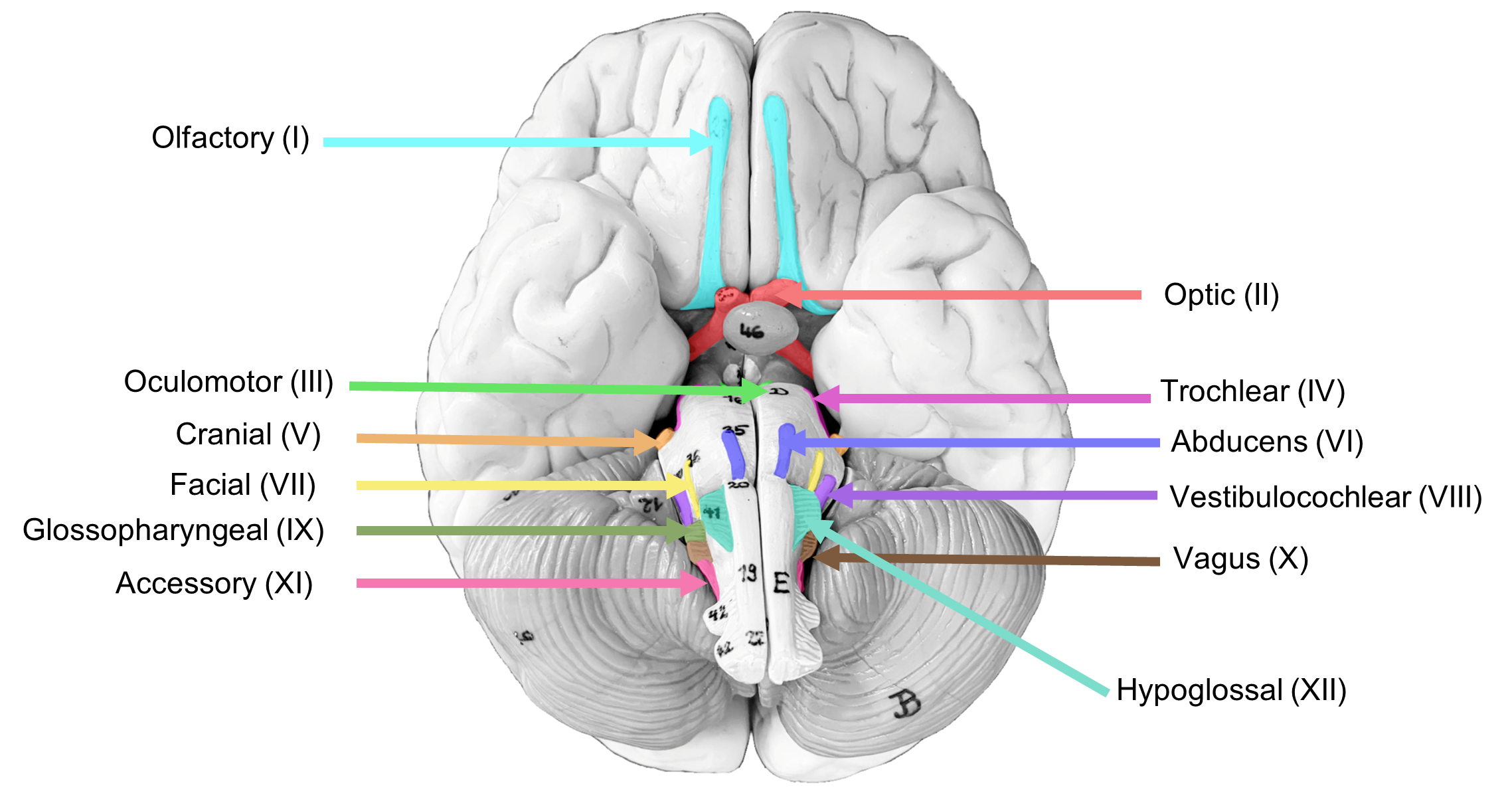
In this activity, you will examine the location of the most prominent cranial nerves and evaluate their functions. There are twelve pairs of cranial nerves, numbered 1-12, based on their attachment point on the left and right sides of the inferior side of the brain (forebrain, mid brain or hindbrain) (Figure 12). Note that cranial nerve I (Olfactory) is at the anterior end of the inferior side of the brain, and that cranial nerve XII (Hypoglossal) is at the posterior end of the inferior side of the brain.
They are named with both a roman numeral and a specific name. Their names are I. Olfactory, II. Optic, III. Oculomotor, IV. Trochlear, V. Trigeminal, VI: Abducens, VII: Facial, VIII. Vestibulocochlear, IX. Glossopharyngeal, X. Vagus, XI. Accessory, XII. Hypoglossal. These twelve pairs of nerves connect the brain to a variety of other organs in the body. To help you learn the names of the cranial nervers, there are a variety of mnemonics that will help you to learn the cranial nerves in numerical order (Table 2).
Some of the 12 cranial nerves carry only sensory information to the brain, and some carry only motor messages to other parts of the body (particularly the muscles). Some cranial nerves are referred to as “mixed” as some of the neurons in the nerve carry sensory signals and other neurons carry motor output signals. Learning the functions of the cranial nerves requires knowing whether each cranial nerve is “sensory”, “motor” or “mixed function”. Memorizing which cranial nerve carries which type of information requires effort and some help from a mnemonic that can be used once you have learned the names of the cranial nerves in numerical order (Table 3). For example, the trigeminal* nerve is a “mixed” nerve, as it carries both sensory nerve fibers and motor nerve fibers. The trigeminal nerve brings sensory signals from the face and mucus membranes to the cerebrum and supplies motor innervation to the muscles of the mouth involved in mastication (chewing).
Table 2: Mnemonics for the names of the cranial nerves
| I | Olfactory | On | Oh! | Oh |
| II | Optic | Old | Once | Oh |
| III | Oculomotor | Olympus | One | Oh |
| IV | Trochlear | Towering | Takes | To |
| V | Trigeminal | Tops | The | Touch |
| VI | Abducens | A | Anatomy | And |
| VII | Facial | Friendly | Final | Feel |
| VIII | Vestibulocochlear | Viking | Very | Very |
| IX | Glossopharyngeal | Grew | Good | Good |
| X | Vagus | Vines | Vacations | Very |
| XI | Accessory | And | Are | Ahhh… |
| XII | Hypoglossal | Hops | Happening | Hhhhh |
Table 3: Functions of the cranial nerves as Sensory (S), Motor (M) or Both (B).
| I | Some | Sensory |
| II | Say | Sensory |
| III | Marry | Motor |
| IV | Money | Motor |
| V | But | Both |
| VI | My | Motor |
| VII | Brother | Both |
| VIII | Says | Sensory |
| IX | Big | Both |
| X | Brains | Both |
| XI | Matter | Motor |
| XII | More | Motor |
Figure 12: Cranial nerves on the inferior view of the brain.
Procedure:
1. Using the model of the brain and the laminated terminology labels, locate and label the following cranial nerves on the brain model: olfactory, optic, trigeminal, abducens and hypoglossal.
2. Once you have labelled these five cranial nerves on the brain model, ask your instructor to check the model and provide their initials here.
Instructor’s initials for labeled cranial nerves on model: ______________
3. Remove the sticky labels and replace them on the terminology sheet and back in the lab binder.
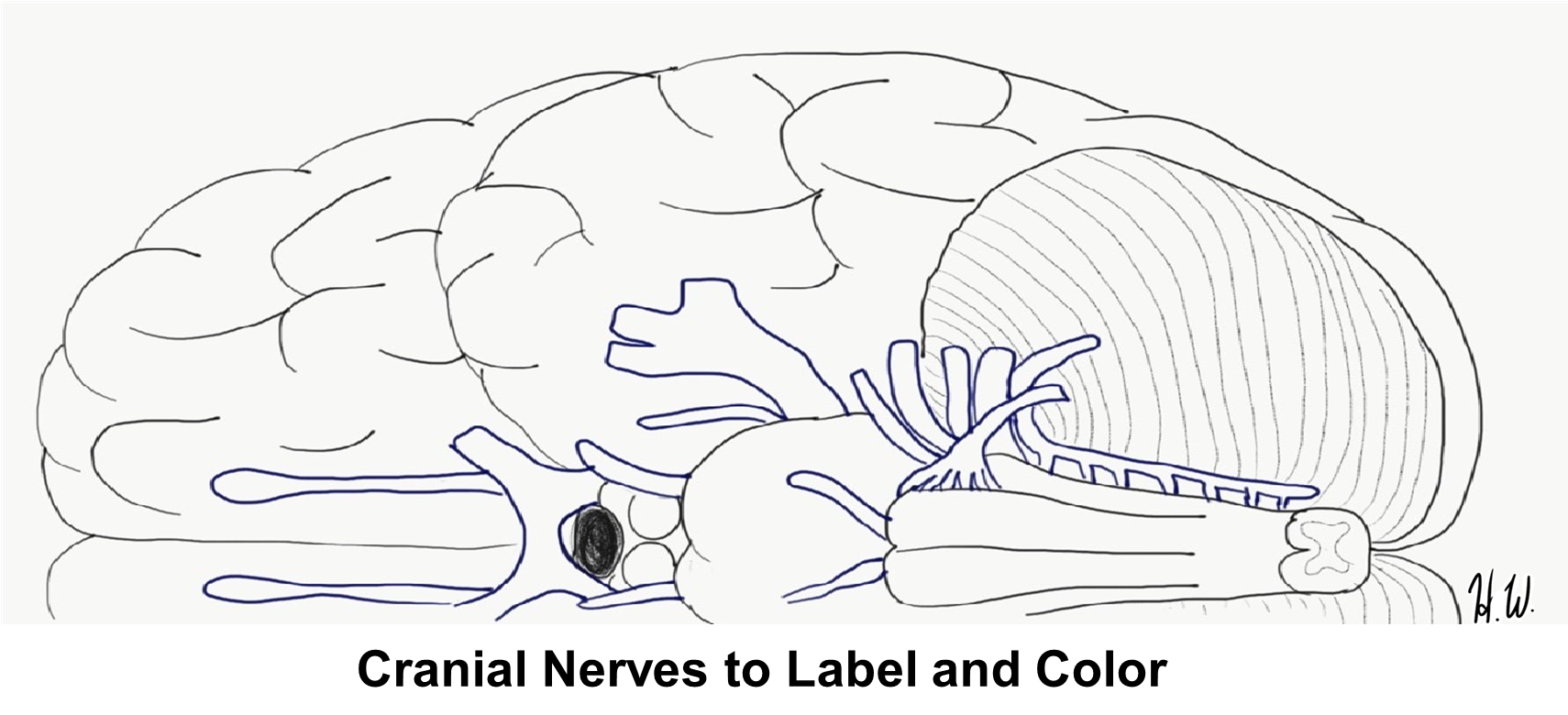
4. Use the image below to label all 12 cranial nerves. Then color all of the sensory nerves red, motor nerves blue and the mixed (both) nerves green.
Cranial Nerves to Label and Color
Activity 5: Evaluation of Cranial Nerve Function
Materials:
- 3-4 cotton balls
- activator
- penlight
- small, labelled vials filled with 3 different scents
- Snellen eye chart
- tuning fork
Background:
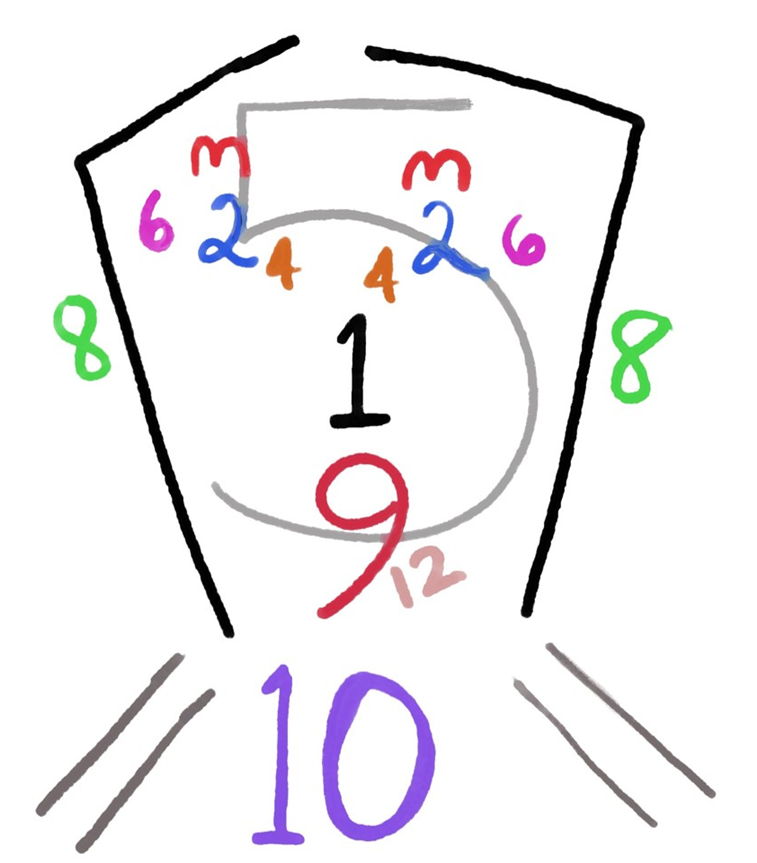
Each cranial nerve innervates a specific region of the body, typically the head and shoulders. One way to learn the different areas innervated by each nerve is by a representative image that depicts the head and shoulders with the numbers of the nerves on the part of the head/neck that is innervated by that nerve (Figure 13).
Figure 13: Representative image of the head and shoulders, indicating which cranial nerve controls what part of the face and shoulders (i.e. CN 3 is located above the eyes because it is responsible for eye movement).
A functional evaluation of the cranial nerves, nerves that attach directly to regions of the brain, is necessary to determine the general location of potential brain injury/damage. By identifying which cranial nerves are not functioning properly, neurologists can determine the location of a brain lesion and the extent of the damage due to the lesion. Cranial nerve assessment can help to assess the next appropriate steps for treatment.
A neurologist can evaluate each of the twelve cranial nerves through a series of non-invasive diagnostic tests. For example, evaluating the olfactory nerve (CN I) is accomplished by waving a small vial of an odor under the patient’s nose, one nostril at a time (Table 4). If the patient can smell and identify the odor, then it is likely the first cranial nerve is intact. Because of Stan’s slurred speech, it is possible that in addition to hydrocephalus, there is a lesion pressing on one or more of the cranial nerves. To become familiar with the tests Stan will undergo, this activity will test your cranial nerve functions.
Table 4: Cranial Nerve Tests
| Nerve | Normal result |
| I (Olfactory) | Identify smell through each nostril |
| II (Optic) | Correctly identify letters on the Snellen chart with each eye |
| III (Oculomotor), IV (Trochlear), VI (Abducens) | Ability to track finger movements up, down, left, right and diagonally, eyelid does not droop |
| V (Trigeminal) | Ability to sense touch on face Jaw should open evenly against resistance and masseter muscles tighten when clenching jaw |
| VII (Facial) | Ability to move facial muscles on both sides of face evenly |
| VIII (Vestibulocochlear) | Ability to hear tuning fork equally in both ears Ability to walk in a straight line without tilting |
| IX (Glossopharyngeal) | Soft palate should move upward when saying “ah” and tongue stays in the mid-line. |
| X (Vagus) | Ability to swallow and speak without hoarseness in voice |
| XI (Accessory) | Rotation of head and contraction of sternocleidomastoid should be obvious Ability to shrug shoulders |
| XII (Hypoglossal) | Ability to extend tongue evenly at the midline and move side to side with equal force |
Procedure:
1. Choose one partner to be the neurologist conducting the test and one partner as the patient undergoing the tests.
Olfactory
2. The patient closes the left nostril while the neurologist has them smell the contents of the 3 vials (one at a time) through their right nostril.
3. Repeat this for the left nostril. If the response is normal, they should be able to smell from each nostril.
4. Write your notes on this cranial nerve test below:
Optic
5. To use the Snellen eye chart, the patient must stand at the mark on the floor (20 feet from the chart). Then have the patient cover their right eye with a cupped hand and read the fourth line of the Snellen eye chart with their left eye.
6. Repeat this for the other eye. If the response is normal, they should be able to see the letters on the chart. The entire chart need not be read.
7. Write your notes on this cranial nerve test below:
Trigeminal
8. After asking the patient to close their eyes, the neurologist tests facial sensation by gently wiping a cotton ball across the frontal region (forehead). If the response is normal, the patient will feel the cotton ball.
9. The neurologist tests motor function by placing their hands on the patient’s masseter muscles (both left and right) and asking them to clench their teeth. If the response is normal, muscle tension is generated equally on both sides.
10. Write your notes on this cranial nerve test below:
Oculomotor, Trochlear, and Abducens
11. Using a penlight 1 foot in front of the patient’s eyes, the neurologist asks the patient to follow the light without moving their head. The neurologist should move the light up, down, left, right and diagonally in both directions. If the response is normal, the patient can track the penlight movements in all directions.
12. Check that the eyelid does not droop.
13. Write your notes on this cranial nerve test below:
Facial
14. The neurologist asks the patient to smile, raise their eyebrows, puff out their cheeks and close their eyes tightly. (Note: we are not performing the taste test that is normally part of this evaluation.) If the response is normal, the patient has symmetrical facial movements.
15. Write your notes on this cranial nerve test below:
Vestibulocochlear
16. Place a cotton ball in the right ear. The neurologist lightly hits a tuning fork against the black rubber activator and holds it up to the left ear of the patient. Move the cotton ball to the left ear and repeat for the right ear. If the response is normal, the patient can hear the tuning fork vibrations in each ear.
17. The neurologist observes as the patient walks in a straight line with one foot in front of the other. This tests balance and the signals relayed from the semi-circular canals in the ear. If the response is normal, the patient can walk in a straight line while keeping their body straight.
18. Write your notes on this cranial nerve test below:
Glossopharyngeal
19. The neurologist asks the patient to say “ah” and yawn. View the tongue and palate. If the response is normal, the tongue should be in the midline and uvula should move symmetrically up and down while saying “ah.”
20. Write your notes on this cranial nerve test below:
Vagus
21. Normally, a test for a successful vagus nerve function would be to assess the gag reflex. We will not test the gag reflex in this evaluation. Instead, the neurologists will ask the patient to swallow and then speak. If the response is normal, the patient can swallow and speak normally without a hoarse (rough) voice.
22. Write your notes on this cranial nerve test below:
Accessory
23. The neurologist places one hand on the right sternocleidomastoid muscle of the patient and another hand on the left side of the patient’s’ head and applies very gentle pressure while asking the patient to turn their head to the left. Repeat for the right side. If the response is normal, the patient can turn the head to both sides equally.
24. The neurologist places both hands on the patient’s shoulders and applies gentle downward pressure while the patient is asked to elevate their shoulders. If the response is normal, the patient can raise the shoulders symmetrically.
25. Write your notes on this cranial nerve test below:
Hypoglossal
26. The neurologist asks the patient to extend their tongue at the midline and then move the tongue side to side. If the response is normal, the patient can move their tongue symmetrically.
27. Write your notes on this cranial nerve test below:
Putting It All Together
Our patient, Stan was diagnosed with hydrocephalus, a condition where a patient develops excess CSF due to inflammation of his meninges, a condition called meningitis. Bacterial meningitis can be treated effectively with intravenous (IV) antibiotics followed by oral antibiotics. Stan is lucky as there are other forms of meningitis caused by fungi or viruses that are less easily treated. He will need to start on a course of antibiotics immediately.
Stan has additional symptoms that cannot be explained by hydrocephalus alone. Evaluate the results from Stan’s cranial nerve tests (Table 5). Use these data to determine which cranial nerve(s) is/are impaired.
Table 5: Results of the patient’s (Stan) cranial nerve function test.
| Olfactory | Can detect odors out of both nostrils | Vestibulocochlear | Hearing normal, slight tilt to the right during walk |
| Optic | Can detect images on Snellen chart | Glossopharyngeal | Swallowing and taste is intact |
| Oculomotor, Trochlear, Abducens | Can track finger movements | Vagus | Normal |
| Trigeminal | Weakness in masseter muscle on right side | Accessory | Slight weakness on right rotation of head |
| Facial | Facial muscle movements limited on right side | Hypoglossal | Tongue drifts to right |
Procedure:
1. View the results of Stan’s cranial nerve function tests (Table 5) and circle the nerve(s) with abnormal function(s)
2. Given the location of the nerves listed above, which general region and on what side of the brain is the probable location of the patient’s lesion? Remember that the left half of the brain controls the right side of the body! Be sure to explain your answer.
Creative Commons Citations:
- Brain and Cranial Nerves, Case-Study Based OER Lab Manual for A&P I © 2022 by G. Backus, H. Wangerin, P. Rodgers is licensed under CC BY-NC-SA 4.0.
- Figures 1, 2, 3, 4, 7, 8, 9. 10, 11, 12 Brain Functional Areas, CSF Flow to Label, and Cranial Nerves to Label and Color © 2022 by H. Wangerin is licensed under CC BY-NC-SA 4.0.
- Figures 5 and 6 © 2023 OpenStax Anatomy and Physiology 2e is licensed under CC BY 4.0.
- Figure 13 © 2022 by G. Backus is licensed under CC BY-NC-SA 4.0.

