7 Introduction to Bones Lab
"To succeed in life, you need three bones: a wish bone, a back bone, and a funny bone." -Reba McIntyre
Gillian Backus; Heidi W. Wangerin; and Paula Rodgers
Objectives
- Identify the parts of a long bone.
- Differentiate among the types of cartilage based on their morphology, location, and/or function.
- Compare and contrast the structure, function, and location of compact and spongy bone.
- Identify the structures of an osteon from an image, model, or microscope slide.
- Trace the flow of nutrients through compact bone using appropriate terminology from an external blood vessel to an individual lacuna (and osteocyte).
- Explain the organic and inorganic components of the extracellular matrix of compact bone and briefly describe the function of each.
Terminology Checklist
Types of Cartilage
|
Anatomy of a Long Bone
|
Microscopic Anatomy of the Osteon
|
Outline of Lab
Case Study: “The Mysterious Femur Fracture”
Activity 1: Examining the Gross Anatomy of Bones
Activity 2: Examining the Cartilage Associated with Bones
Activity 3: Examining the Histology of Bone
Activity 4: Examining the Components of Bone
Putting it all Together
Case Study: “The Mysterious Femur Fracture”
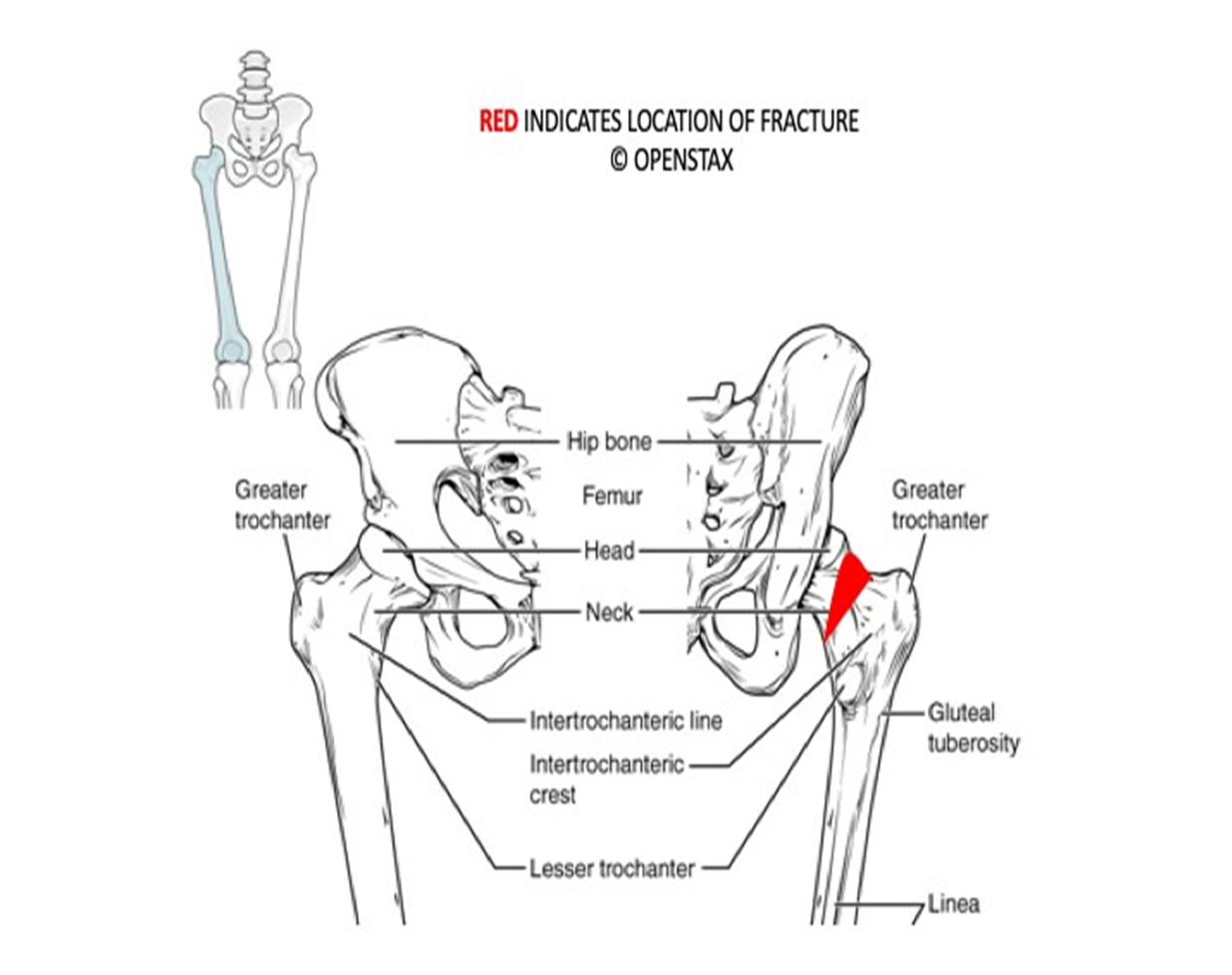
An 86-year-old woman named Therese has been referred to you after fracturing the neck of her left femur (at the greater trochanter, near the proximal epiphysis). She fractured her femur after slipping in the shower (Figure 1). Typically, femurs will only fracture under a tremendous amount of stress. It is unusual that she fractured this bone after a fall from standing height.
Describe the location of the patient’s fracture using the information in the case study and Figure 1.
Figure 1: Fractured neck of the femur bone.
Activity 1: Examining the Gross Anatomy of Bones
Materials:
- none
Background:
Not all bones look like typical dog bones! Bones can be long, short, flat, irregular, or sesamoid. The femur, humerus, ulna, radius, tibia and fibula are good examples of long bones – a bone made of a long shaft with two bumpy ends. Short bones, like the smaller bones of the wrist (carpals), and the smaller bones of the ankle (tarsals) are typically wider than they are long. Flat bones are found mostly in the skull and include the flat plates of the occipital bone, frontal bone, and others. Many bones are irregularly shaped, defying the short, long, or flat definitions. Examples are vertebrae, ribs, scapula, clavicle, and mandible. Sesamoid bones are embedded in tendons. Examples are the patella and hyoid bone.
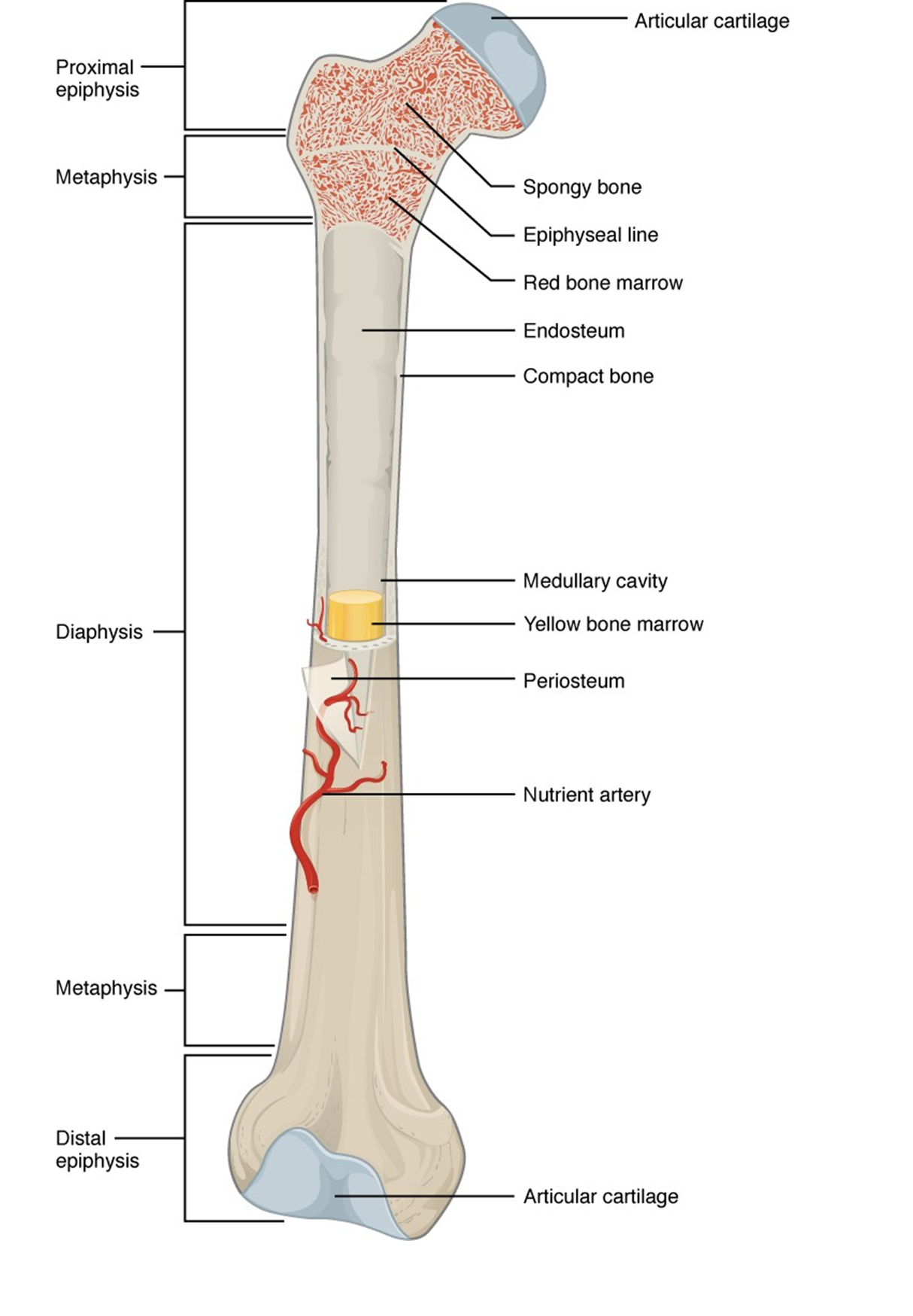
On a typical long bone, the long shaft is called the diaphysis and the bumpy ends are called the proximal and distal epiphyses. Between the epiphysis and the diaphysis is the metaphysis. Depending on the bone’s age, this area can be called the growth plate, or epiphyseal plate. As a child grows, the hyaline cartilage of the epiphyseal plate is gradually replaced by bone. In adulthood, the epiphyseal plate is a remnant of its younger self and is called the epiphyseal line. Once the epiphyseal plate closes, the bone can no longer grow in length. However, the bone can still change in thickness.
As with all organs, bones are made of more than one tissue type. Bones are made of dense fibrous connective tissue, reticular tissue, blood, as well as bone (osseous) tissue. A leathery, dense fibrous connective tissue called the periosteum makes up the most superficial layer. Under the periosteum is the bulk of the bone’s mass, osseous tissue, either compact (cancellous) bone or spongy bone. Because solid bone would be too heavy, the inside of many bones is mostly hollow, the medullary cavity. The outer layer of the medullary cavity, called endosteum, contains a layer of bone forming and bone resorbing cells. The rest of the medullary cavity is filled with reticular tissue called bone marrow. There are two types of bone marrow: yellow marrow, which stores fat, and red marrow, which produces red blood cells, white blood cells, and platelets (Figure 2).
Figure 2: Anatomy of a long bone.
Procedure:
- Describe the difference in location between the periosteum and the endosteum.
- Sketch a typical long bone and label: diaphysis, epiphysis, articular cartilage, medullary cavity, epiphyseal plate, periosteum, and endosteum.
Activity 2: Examining the Cartilage Associated with Bones
Materials:
- microscope (one per student)
- microscope slides of hyaline cartilage, fibrocartilage, and elastic cartilage
Background:
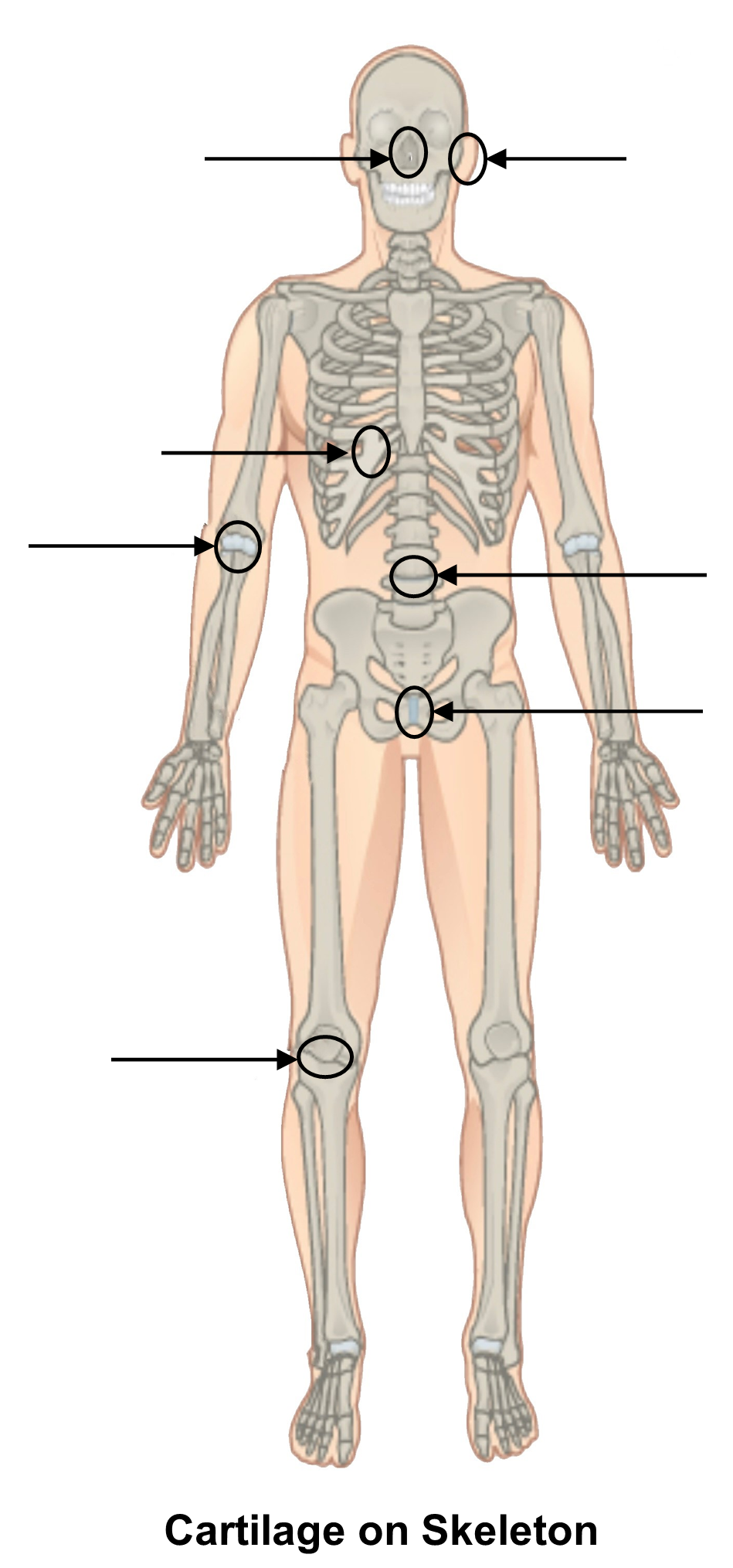
In addition to osseus (bone) tissue, another tissue type commonly associated with bone is its sturdy but squishier cousin, cartilage. There are three types of cartilage: hyaline, elastic, and fibrocartilage (Figure 3). Hyaline cartilage is softer than fibrocartilage and is located at the end of each bone (called articular cartilage), where it provides a smooth joint surface for bones to rub against each other; hyaline cartilage is also found at the epiphyseal plate, where the cells divide readily and allow bones to grow in length until post puberty. The hyaline cartilage that connects the ribs to the sternum is called costal cartilage. Hyaline cartilage also forms the fleshy lower part of the nose.
Figure 3: Microscopy (right) and drawings (left) of three types of cartilage.
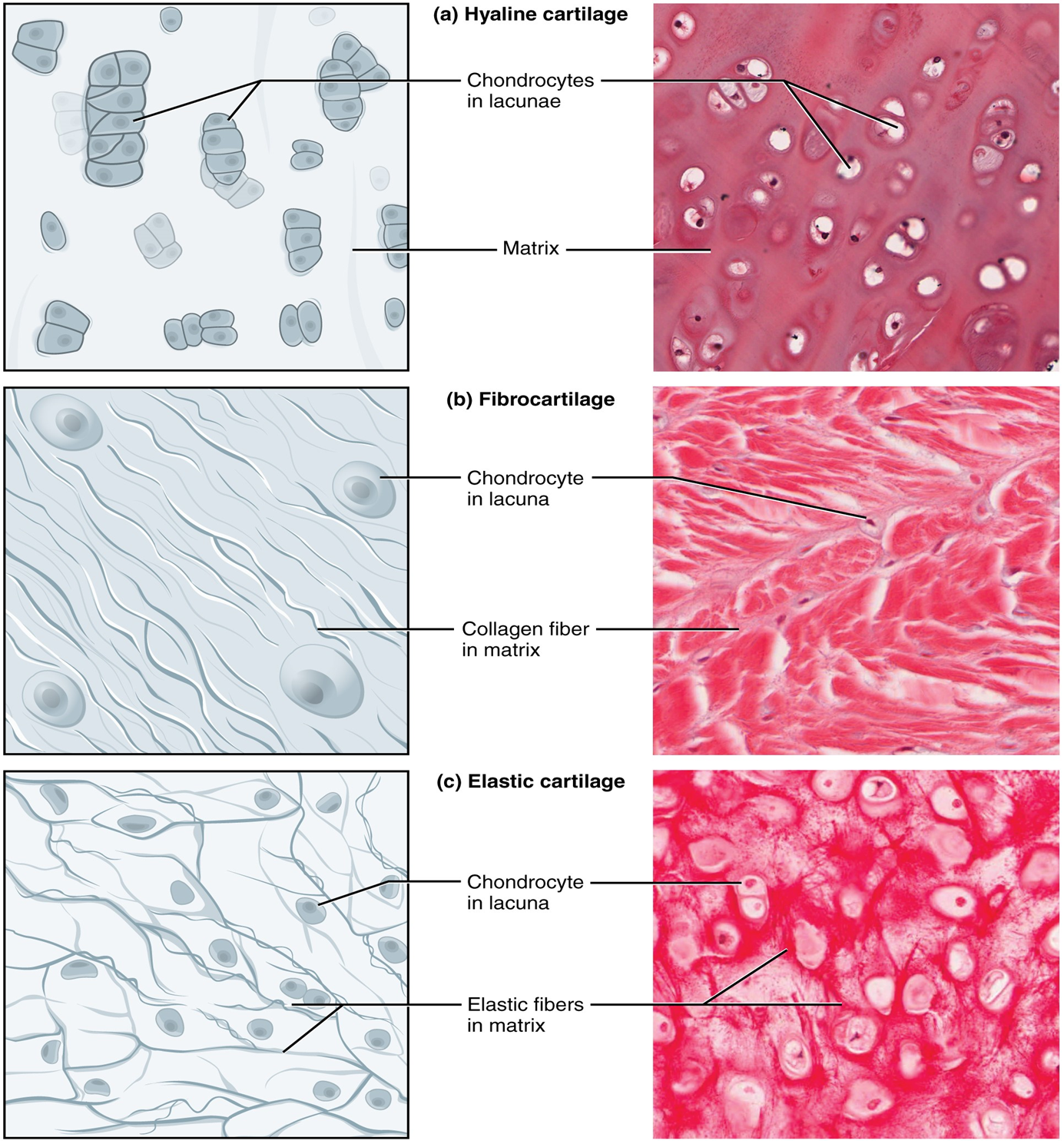
Fibrocartilage contains not only a cartilage matrix but also a great deal of collagen fibers to provide extra support. This type of cartilage resists compression better than hyaline cartilage. The embedded collagen fibers make it sturdier. Fibrocartilage makes up the intervertebral disks (between the vertebrae bones), the pubic symphysis (between the pubic bones), and the meniscus of the knee.
The third type of cartilage is elastic cartilage. It forms the pinna, the outer portion of the ear, and the epiglottis which sits above the trachea and prevents food from entering the respiratory tract when swallowing. Rather than tough collagen fibers, elastic cartilage is supported with a network of elastic fibers. Feel your ear to remind you how springy, yet tough this cartilage is.
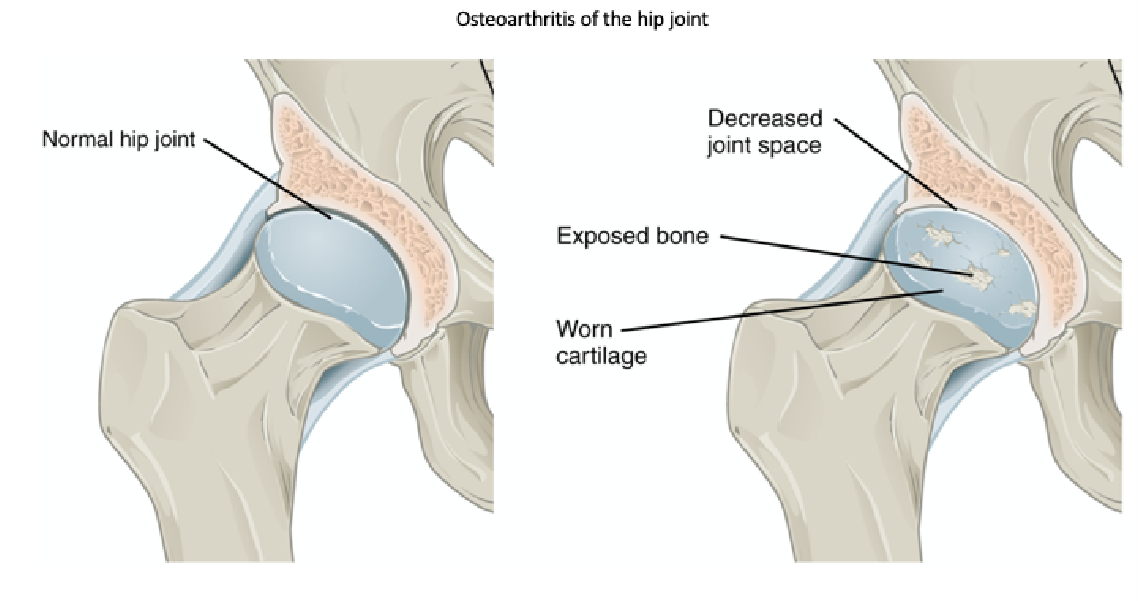
Therese’s radiograph reveals that the space between the head of the femur and the hip joint (acetabulum) is narrowed, indicating that the hyaline cartilage at the epiphysis of the femur has worn away, reducing the cushioning ability of the hip joint (Figure 4). In severe cases, no hyaline cartilage may remain in places, making bone rub against bone. Thinning of the articular cartilage typically occurs with age but can be exacerbated by improper diet or excessive wear and tear and is called osteoarthritis.
Figure 4: Head of the femur and its articulation with the pelvis showing the presence of exposed bones due to osteoarthritis.
Procedure:
1. Use the reading to review where you would find the three distinct types of cartilage on a skeleton. Then, label the different types of cartilage on the image of the skeleton below.
2. Use Figure 3 to identify and label the several types of cartilage visible under a microscope.
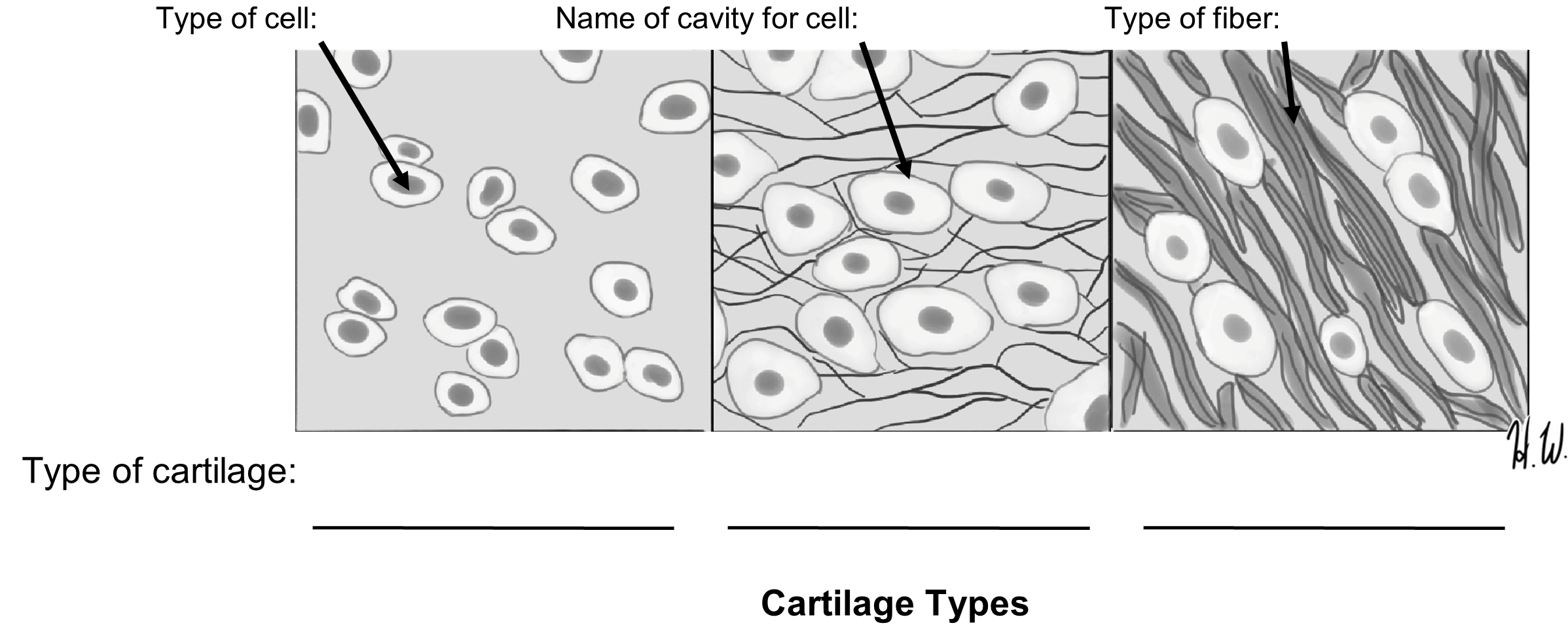
3. As time permits, review the three types of cartilage under the microscope, using high power (40x, blue) to be sure you can reliably recognize each.
4. Our patient has injured cartilage. Use Figure 4 to identify the type of cartilage that was damaged.
Activity 3: Examining the Histology of Bone
Materials:
- model of an osteon and/or laminated image of the model
- terminology labels with sticky tack
Background:
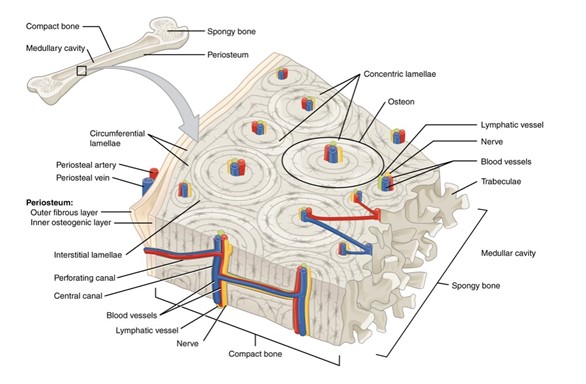
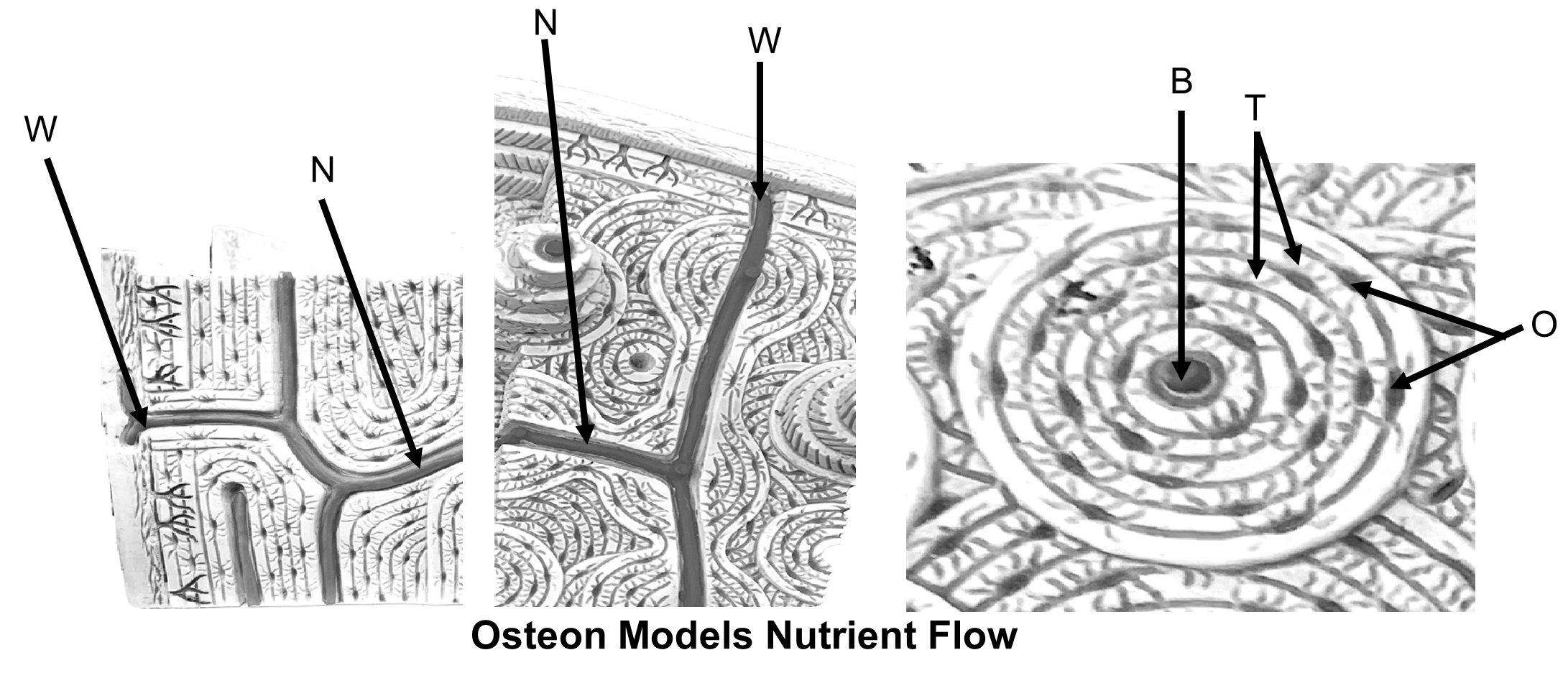
When we look at bone under a microscope, we notice that there are two types of bones: compact (or cancellous) bone and spongy bone. Compact (cancellous) bone is found at the edges of bone and consists of circular, tree-trunk shaped units called osteons (Figure 5). Each osteon consists of rings of tissue surrounding a central canal that holds blood vessels and nerves. The tiny osteocytes, located in cavities called lacunae, are in the concentric rings called lamellae surrounding the central canal. There are also tiny radiating canals called canaliculi emanating from the central canal that deliver nutrients to the lacunae.
For an osteocyte to receive nutrients and get rid of waste, it must be serviced by a series of blood vessels. Blood vessels enter bone via the nutrient foramen where they wind their way among the bone tissue via horizontal Volkmann’s (or perforating) Canals. These horizontal canals intersect with vertical central canals that serve the center of each osteon. From there, the tiny canaliculi distribute blood from the central canal to the lacunae.
Figure 5: The organization of compact bone into osteons.
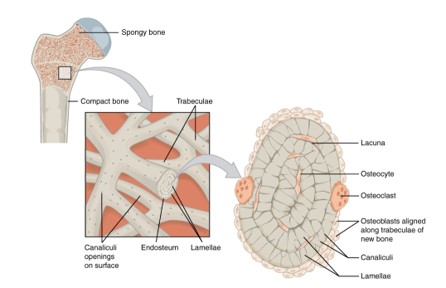
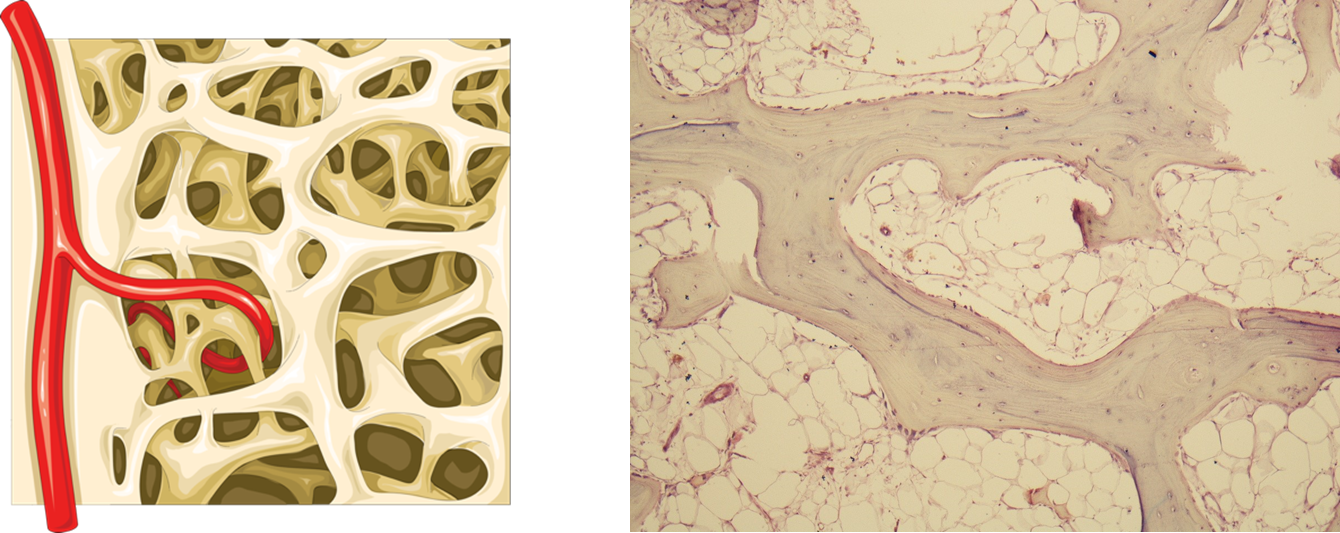
Spongy bone has a less rigid arrangement than compact bone and looks like Swiss cheese. It is organized into randomly arranged columns called trabeculae covered by a thin layer of endosteum (Figure 6). In between the interwoven trabeculae are spaces filled with red bone marrow. Spongy bone trabeculae contain lacunae and canaliculi but lack a central canal. In spongy bone, nutrients diffuse across the endosteum and from cell to cell directly, rather than being distributed via the central canal.
Figure 6: The organization of spongy bone into trabeculae.
Procedure:
1. Using the models available in lab, label the osteon model. Leave your model labelled on your lab bench until the end of activity 3.
2. Label the trabeculae on the image and histology image of the spongy bone below.
3. Determine how a single osteocyte receives nutrients by putting the letters in order. Start from how the blood comes into the bone and ends at the bone cell. List the letter and names of the corresponding structures. Use the labeled model to help you label the images appropriately.
| Order | Letter | Structure |
| 1 | ||
| 2 | ||
| 3 | ||
| 4 | ||
| 5 | O | Osteocyte |
4. Once you have completed this activity, have your instructor check your labeled model and the answers to the above questions and get their initials.
Instructor initials for labeled model and activity_______________________
5. Remove the labels from the model and neatly return them to their sheet.
Activity 4: Examining the Components of Bones
Materials:
- acid-soaked chicken bone in a bag
- baked chicken bone in a bag
- fresh chicken bone in a bag
Background:
Therese is questioned about her medical history. She went through menopause between ages 50-54. As women age and enter menopause starting around age 50, estrogen levels fall leading to a condition called osteoporosis. This can lead to a decrease in bone density. A bone density test could help to explain how an insignificant impact could lead to a significant fracture.
Bone tissue is comprised of 65% inorganic and 35% organic material. The inorganic minerals provide strength and rigidity to the bone and is composed primarily of hydroxyapatite crystals which is, in turn, mostly made of calcium. The organic matrix, or osteoid, is composed of collagen, a protein that provides elasticity and resistance to twisting. The two cells responsible for building and breaking down the bone matrix are osteoblasts and osteoclasts, respectively. Estrogen inhibits the activity of osteoclasts preventing the breakdown of the bone matrix. Estrogen levels and collagen production decrease with age causing a weakening of the bony matrix and loss of bony density. This can reduce bone remodeling and reduce the ability of bone to withstand impact.
In this activity we will observe the effects of these two components of bone: the inorganic component, calcium, and the organic component, collagen, by subjecting raw chicken bones to two different conditions. One bone will be baked. Heating the protein found in bone, collagen, causes it to denature or unravel such that the strong collagen fibers weaken. This makes the bone more brittle, compared to a raw bone that still has its collagen skeleton intact. The other bone will be soaked in acid, which will leach out the calcium.
Procedure:
1. Find the tray with the raw, acid soaked, and baked bone, and fill in the table below. Pick up the bones with your gloved hands and compare their texture and flexibility. Fill in the table below.
| Raw Bone | Acid-Soaked Bone | Baked Bone | |
| Observations on texture | |||
| Component missing in bone matrix | Nothing missing (normal) |
Putting It All Together
Therese will require surgery to help the bone heal, due to her fracture type and age Before surgery, however, she is sent for a full blood work-up (Table 1) to establish a possible cause for her decrease in bone density.
Table 1: Blood work values for Therese
| Calcium level | Estrogen level | |
| Patient | 4.6 mg/dL | 5 pg/mL |
| Normal | 8.6-10.3 mg/dL blood (UCLA) | >10 pg/mL |
Procedure:
1. Compare the patient values with the normal values in Table 1. Are these values high or low, compared to normal?
2. Be sure you understand these values’ meaning before leaving the lab as you will answer questions in the post-lab about these differences.
Creative Commons Citations:
- Introduction to Bones Lab. Case-Study Based OER Lab Manual for A&P I © 2022 by G. Backus, H. Wangerin, P. Rodgers is licensed under CC BY-NC-SA 4.0.
- Figures 1, 2, 3, 4, 5, and 6, and Cartilage on Skeleton © 2023 OpenStax Anatomy and Physiology 2e is licensed under BB BY 4.0.
- Cartilage Types, Spongy Bone Histology to Label, Osteon Models Nutrient Flow, Cartilage Histology, Spongy Versus Compact Bone © 2022 by H. Wangerin is licensed under CC BY-NC-SA 4.0.
- Spongy Bone to Label © 2019 Laboratories Servier under CC BY-SA 3.0.

