6 Integument Lab
"And forget not that the earth delights to feel your bare feet and the winds long to play with your hair." -Khalil Gibran
Gillian Backus; Heidi W. Wangerin; and Paula Rodgers
Objectives
- Identify the specific tissue type and explain the function of each layer of the epidermis, dermis, and hypodermis.
- Identify, label, and define the function of the structures of the integument from a model or image.
- Identify the layers of the epidermis and dermis from a microscope slide.
- Explain the function and location of the different structures and cells of the epidermis, dermis, and hypodermis.
- Differentiate between thick and thin skin based on appearance, structure, and function.
Terminology Checklist
*Indicates structures you will need to identify under a microscope as well as on a model or images
Layers of the epidermis
|
Structures of the skin
|
Cells of the epidermis
|
Types of skin
|
Outline of Lab
Case Study: “Cancer is Only Skin Deep”
Activity 1: Layers and Cells of the Epidermis
Activity 2: Layers and Structures of the Dermis and Hypodermis
Putting It All Together
Case Study: “Cancer is Only Skin Deep”
As a nurse working in a dermatology office, you see patients who come into the office with various nodules, lesions, and rashes that need to be imaged and/or biopsied to test if they are cancerous. This afternoon a middle-aged female walks into the office with a flat, scaly sore on her leg. The patient has several risk factors for skin cancer including using tanning beds in her teenage years and having fair skin. You meet with the patient and make several visual observations of the lesion as well as record her medical history. You mark the location of the lesion on the leg (Figure 1) and take a close-up image of the features and size of the lesion (Figure 2). You biopsy a small piece of the lesion to send to the lab to test for the presence of cancer cells.
Using correct anatomical surface terminology as well as two directional terms, describe the location of the lesion on the patient’s leg.
Figure 1: Representative image of the human body with the location of the lesion on the body of the patient marked with an X.

Figure 2: Image of lesion on patient’s leg.

Activity 1: Layers and Cells of the Epidermis
Materials:
- dropper bottle of isopropyl alcohol
- lens paper
- microscope
- microscope slide of thick skin (sole of foot)
- microscope slide of thin skin (scalp, or skin with hair follicles)
Background:
The skin is the largest organ in the body. The many functions of integument include sensation, protection, and regulation. Many different structures in the skin help to carry out these various functions, including sensory receptors, muscles and glands. The skin itself is made of the epidermis, the outer layer of stratified squamous epithelial cells which is about 0.1 mm thick, and the dermis, the deeper layer which is about 4 mm thick. Below these two layers of skin is a deeper layer of connective adipose tissue called the hypodermis. This layer serves to anchor and connect the skin to the underlying organs.
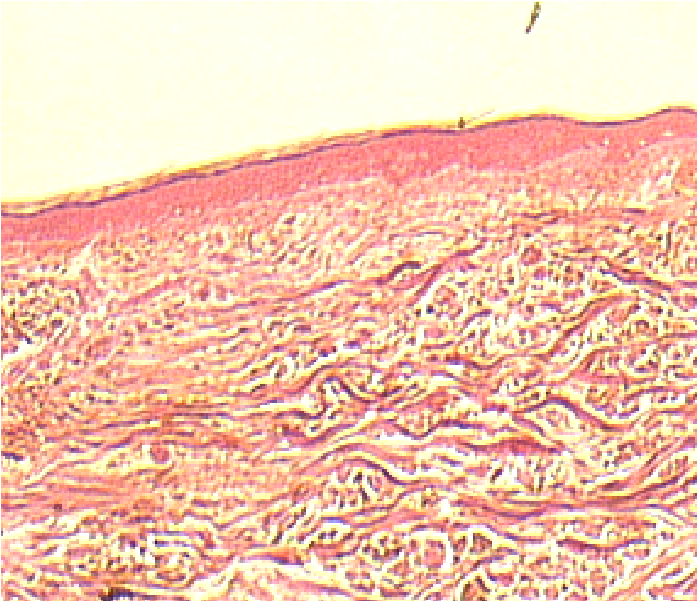
The epidermal layer is composed of four to five layers of stratified squamous epithelium depending on location on the body. The bottom or deepest layer is the stratum basale, followed by the stratum spinosum, stratum granulosum, stratum lucidum, and stratum corneum (Figure 3 and 4).
Figure 3: Slide of thick skin
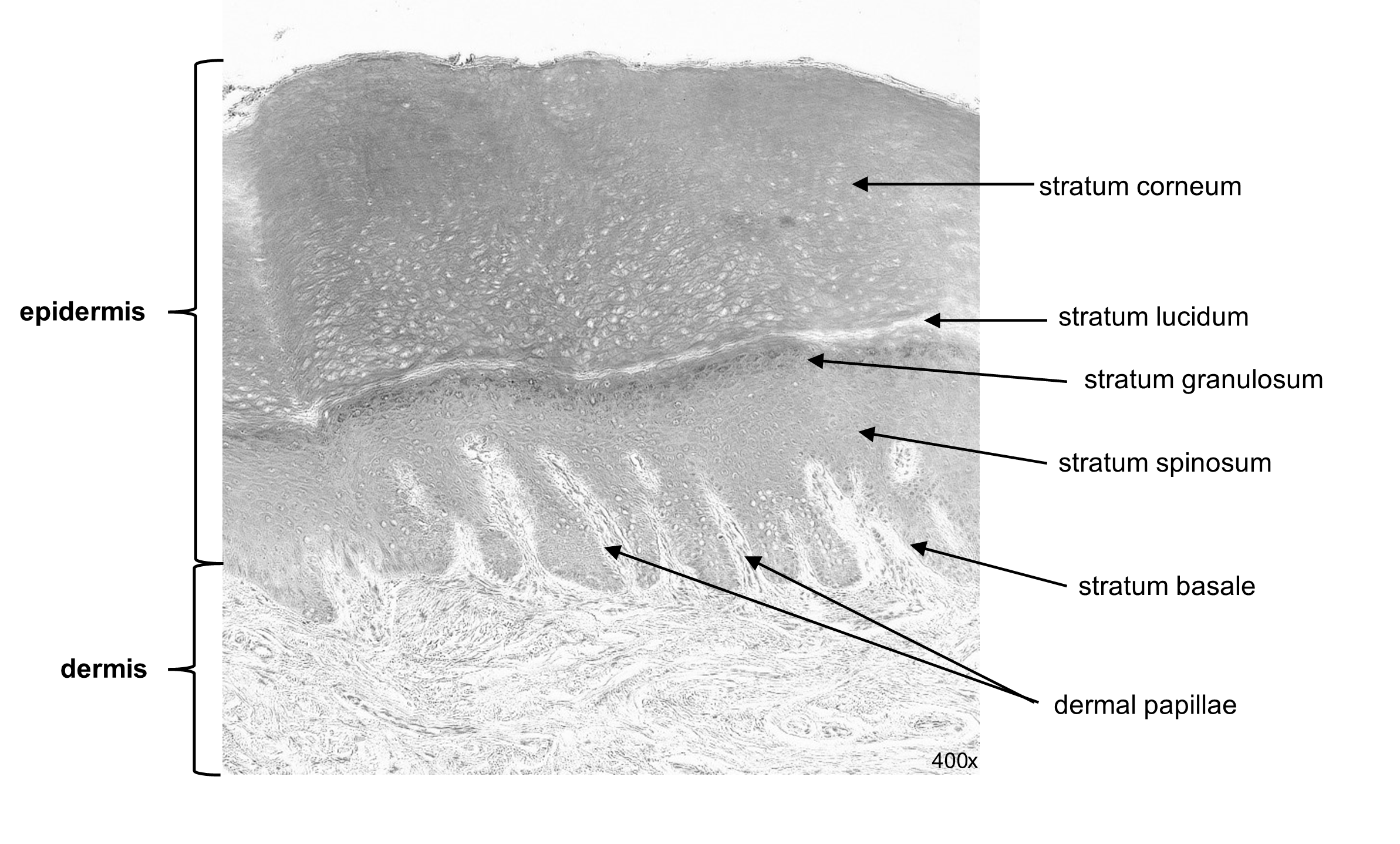
The deepest layer of the epidermis is the stratum basale. It consists of a single layer of mitotically active cells that are continuously replacing sloughed off skin cells. They are separated from the dermis by the basement membrane. Nutrients diffuse across the basement membrane from the dermis into the epidermis. When the basale cells divide out of control, the result is a form of skin cancer called basal cell carcinoma. Just superficial to the basale layer, there are 8 to 10 rows of epithelial cells that comprise the stratum spinosum. These spindle shaped cells accumulate quantities of pre-keratin protein and are therefore known as keratinocytes. As the keratinocytes mature, they are pushed into the next layer by cells emerging from the stratum basale layer. When these cells are overabundant, the diagnosis is squamous cell carcinoma. The next layer, the stratum granulosum, consists of 3-5 rows of epithelial cells and is the final layer to permit the diffusion of nutrients from the dermis. Beyond the stratum granulosum is the most superficial layer, stratum corneum. These dead keratinocytes are filled with the protein keratin and are waterproof. This layer thus provides protection and prevents water loss.
In thick skin there is an additional thin layer between the stratum corneum and stratum granulosum called the stratum lucidum. It stains faintly and appears clear or translucent on a microscope slide. There are some regions of the body where the epidermis is naturally thicker, notably in the soles of the feet and the palms of the hands, places that are more subject to abrasion. Thick skin has many more rows of cells, including a thicker stratum corneum, and the presence of the stratum lucidum (Figure 3). All other regions of the body feature thin skin. Thin skin lacks the stratum lucidum layer and has fewer rows of cells in the stratum corneum. Thin skin also has hair follicles and is sometimes referred to as “hairy skin.”
Most of the skin is composed of keratinocytes, but other cell types occupy the five epidermal layers, including melanocytes and tactile cells. Melanocytes contain the protein melanin, a pigment which gives skin its color and tone. Interestingly, all humans have a similar number of melanocytes, regardless of their skin tone. What makes a person darker or lighter is the quantity and concentration of pigment protein within the cells. When melanocytes become cancerous, the diagnosis is called melanoma. Tactile cells or Merkel cells are in the stratum basale and detect sensation of light touch.
Figure 4: Layers of the epidermis.
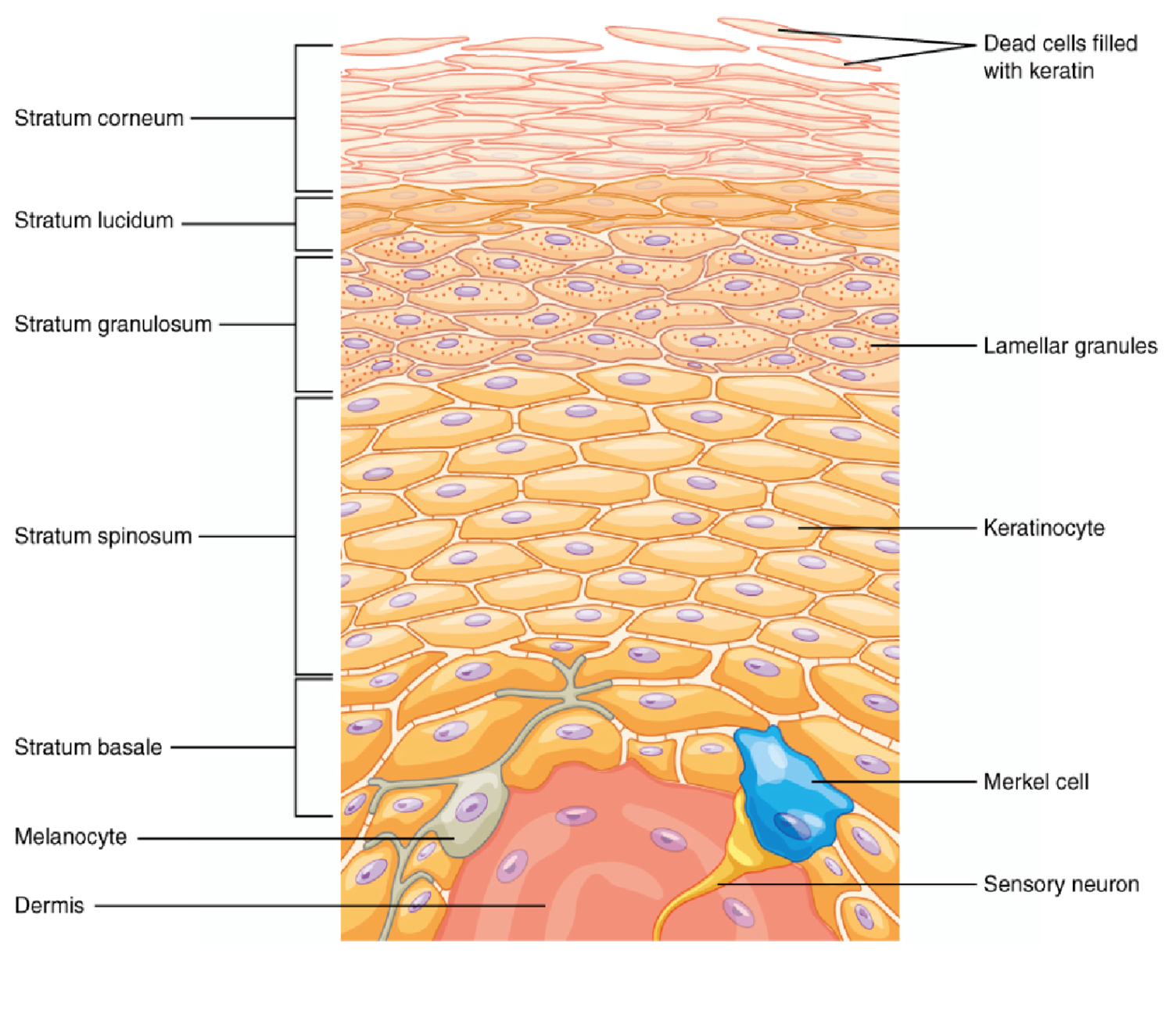
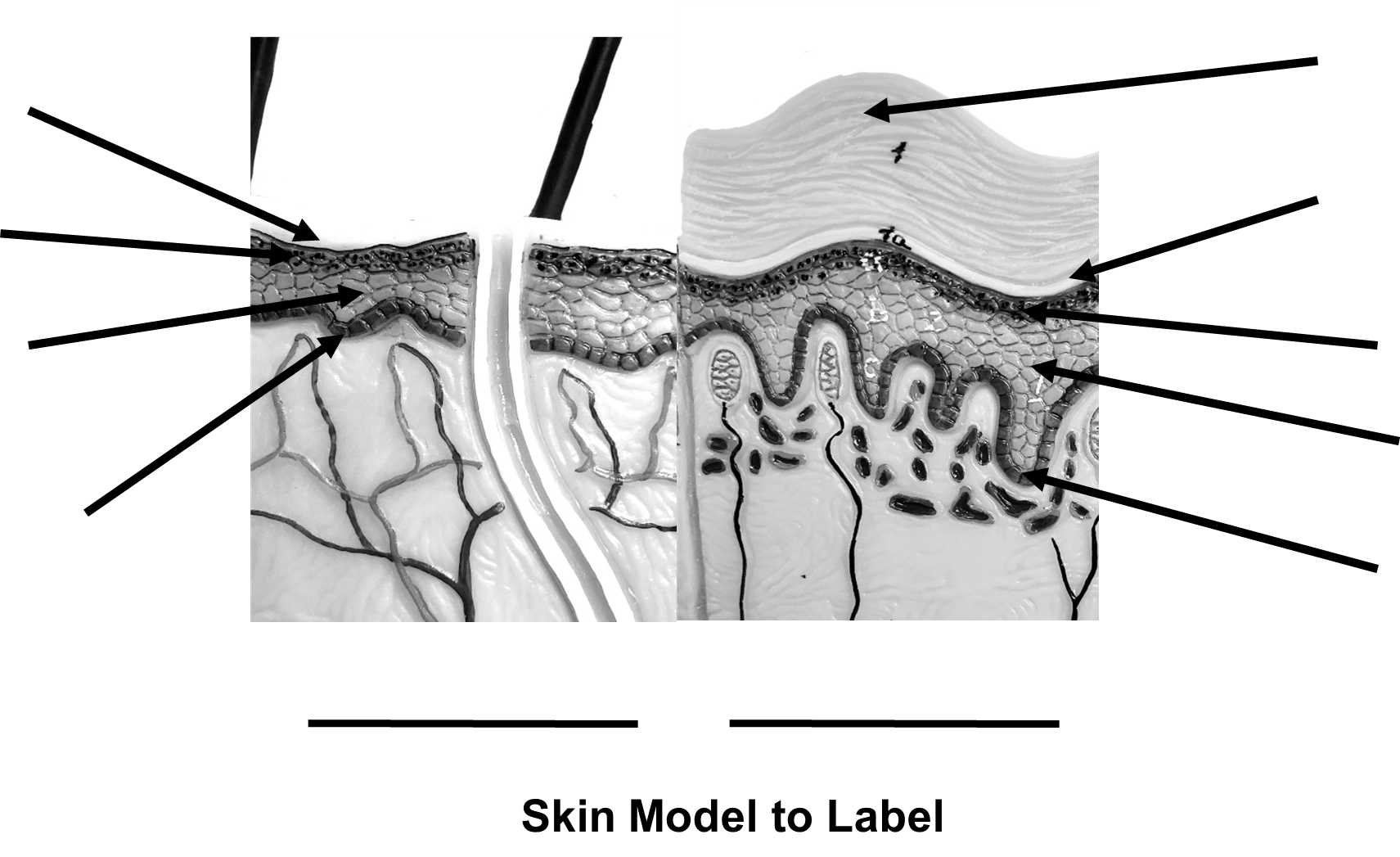
Procedure:
1. On the two side-by-side images of the skin model, label which image represents thick skin and which represents thin skin. Label the layers of each (arrows).
2. View the slide of thick skin (sole of foot) under the microscope at high power (40x, blue) and locate the five different layers of the epidermis.
3. In the space below, make a representative scientific drawing of the epidermis of thick skin and label the five layers of the epidermis: stratum basale, stratum spinosum, stratum granulosum, stratum lucidum, and stratum corneum.
4. View the slide of thin skin (scalp) under the microscope at the high power objective (40x, blue) and locate the four different layers of the epidermis.
5. In the space above, make a representative scientific drawing of the epidermis of thin skin and label the four layers of the epidermis: stratum basale, stratum spinosum, stratum granulosum, and stratum corneum. (Leave the slide of thin skin on the microscope for Activity 2.)
6. Write down three visible differences between the slide of the thick and thin skin.
-
- _________________________________
- _________________________________
- _________________________________
Activity 2: Layers and Structures of the Dermis and Hypodermis
Materials:
- dropper bottle of isopropyl alcohol
- lens paper
- microscope
- microscope slide of thin skin (scalp, hair with follicle)
- skin model
- terminology labels with sticky tack
Background:
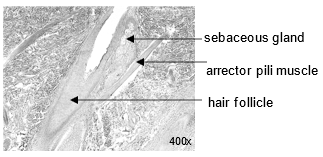
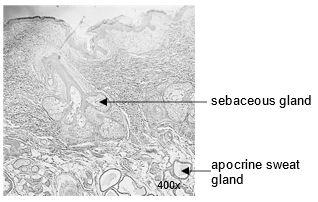
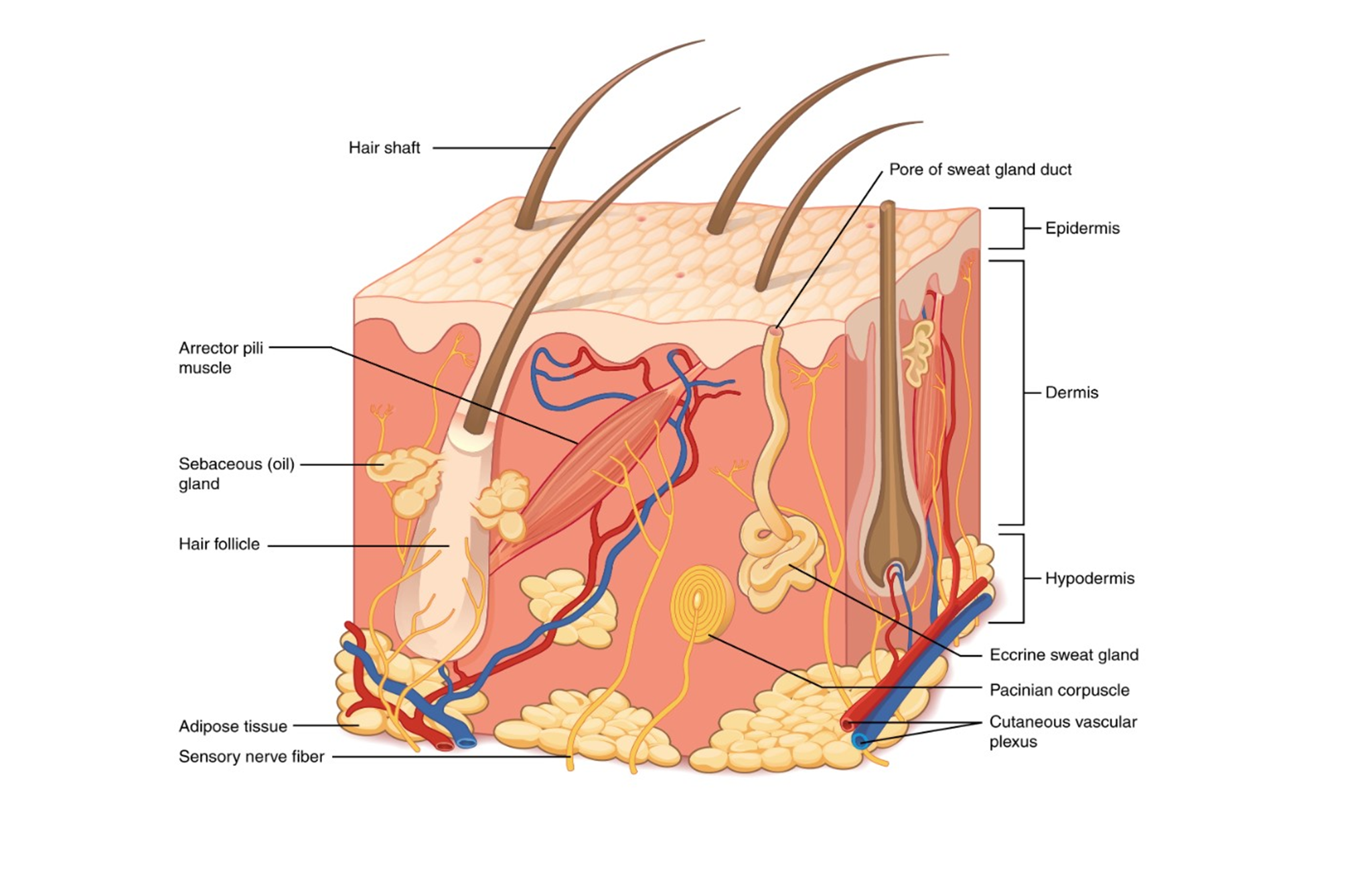
The skin is made of more than just the epidermis. Deep to the epidermis lies two additional regions: the dermis and the hypodermis. The dermis is located below the basement membrane and has two layers. The papillary layer is a thin layer of loose areolar connective that projects finger-like dermal papillae that support the epidermis (Figure 3). The reticular layer is much thicker and contains dense irregular connective tissue. The dermis contains many collagen fibers running in different directions, giving the skin tensile strength and some elastic fibers to provide some elasticity. Resident cells include fibroblasts, and macrophages. The dermis also contains blood vessels which bring nutrients to the epidermal cells, as well as house nerve endings for sensation. Embedded in the dermal tissue are the sweat (sudiferous) glands, oil (sebaceous) glands, and hair follicles. The eccrine sweat glands help to regulate temperature, the sebaceous glands assist in waterproofing the skin’s surface, and the hair follicles produce the hair that protrudes from thin skin (Figure 5 and 6). Arrector pili muscles contract to erect hairs giving the appearance of goose bumps which are thought to help increase the insulating layer of warm air near the skin.
| Figure 5: Hair follicle.
|
Figure 6: Glands of the skin.
|
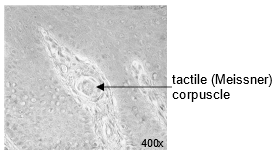
Figure 7: Tactile (Meissner) corpuscle
|
Apocrine sweat glands are larger than eccrine sweat glands and make a viscous sweat that bacteria break down to produce an odor (Figure 6). Apocrine sweat glands are typically found in the axillary and genital regions and secretions are released into the hair follicle directly.
The dermis of the skin is full of specialized sensory nerve structures. Tactile (Meissner) corpuscles respond to light touch and can be found in the dermal papillae (Figure 7). Lamellated (Pacinian) corpuscles respond to vibrations and are found in the reticular layer.
Under the dermis lies the hypodermis. This is a layer of adipose tissue for insulating the skin (Figure 8). When you receive a sub-dermal or sub-cutaneous (“SubQ”) injection, the needle is inserted in this fatty tissue.
Figure 8: Image of the structures of the skin.
Procedure:
1. Use the skin model and the provided labels to locate each structure on the skin model listed on the terminology checklist under “Structures of the Skin”.
2. Show the complete, labeled model to your instructor and have them sign below.
Labeled Skin Model Instructor’s initials ___________
3. Remove the labels from the model and place them back on the terminology sheet.
4. View the slide of thin skin (hairy skin, scalp, hair with follicles) under the microscope using scanning power (4x, red). Name the tissue type associated with the epidermis, the dermis, and the hypodermis and complete the table below:
| Layer | General Tissue Category (epithelial, connective, muscle or nervous) | Specific sub-type of tissue |
| Epidermis | ||
| Dermis | ||
| Hypodermis |
Putting It All Together
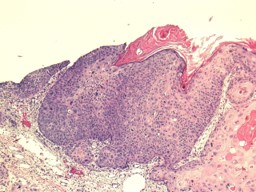
Now that you have learned to identify and explain the functions the different layers of the skin as well as the structures found in each of these layers, you can now apply this knowledge to an abnormal biopsy of the skin. The biopsy was returned from the lab (Figure 9); it is your job to describe the histological features of the lesion. The dermatologist has identified abnormal looking cells which indicate skin cancer.
1. On Figures 9 and 10 below, please label the epidermis and the dermis (hint: look for the stratum basale and the basement layer).
| Figure 9: Biopsy of acute squamous cell carcinoma.
|
Figure 10: Normal thin skin (for comparison).
|
2. This biopsy was taken from the patient’s leg, and therefore is thin skin. Describe how the biopsied skin appears abnormal from what you would expect from normal thin skin.
Creative Commons Citations:
- Integument Lab, Case-Study Based OER Lab Manual for A&P I © 2022 by G. Backus, H. Wangerin, P. Rodgers is licensed under CC BY-NC-SA 4.0.
- Figure 1 © 2022 by P. Rodgers is licensed under CC BY-NC-SA 4.0.
- Figures 2, 4, and 8 © 2023 OpenStax Anatomy and Physiology 2e is licensed under BB BY 4.0.
- Figures 3, 5, 6, 7 and 10 © 2022 by H. Wangerin is licensed under CC BY-NC-SA 4.0.
- Skin Model to Label © 2022 by G. Backus, H. Wangerin, P. Rodgers is licensed under CC BY-NC-SA 4.0.
- Figure 9 © 2022 by Dr. J. Bragg is licensed under CC BY-NC-SA 4.0.