5 Histology Lab
"The most alarming moments of anatomy are not the bizarre, the unknown. They are the familiar." -Christine Montross
Gillian Backus; Heidi W. Wangerin; and Paula Rodgers
Objectives
- Locate and identify from an image or histology slide the diverse types of epithelial tissue.
- Describe the function and common locations of the diverse types of epithelial tissue.
- If applicable, describe the structural modifications (cilia, microvilli, or keratinization) that contribute to the specific function of each epithelial tissue sub-type.
- Locate and identify from an image or histology slide the several types of connective tissue (11 types).
- Describe the function and common locations of the diverse types of connective tissue.
- On an image or histology slide of connective tissue, identify the ground substance and the diverse types of protein fibers that create the extracellular matrix of connective tissue.
- Describe how protein fibers and ground substance contribute to the function of the different connective tissue types.
- On a picture or histology slide of connective tissue, identify the most common type(s) of cells present.
- Differentiate between the three types of cartilage.
- Locate and identify from an image or histology slide the 3 distinct types of muscle tissue.
- Describe the function and common locations of the 3 diverse types of muscle tissue.
- On an image or histology slide, identify nervous tissue.
- Explain the several types of tissue in an organ and how they contribute to the organ’s function.
*By the end of this lab you should have an idea of the typical pattern each tissue has. Do not try to memorize a set image of the tissue types but try to understand the function of a tissue and how it would relate to its morphological features.
Terminology Checklist
Terminology for Epithelial Tissue
|
Types of Epithelial Tissue
|
Terminology for Connective Tissue
|
Types of Muscle Tissue
|
Nervous Tissue
|
Outline of the Lab
*Note: This lab may be divided into two sections & completed in two weeks.
Case Study: “Case of the Persistent Cough”
Activity 1: Epithelial Tissue
Activity 2: Connective Tissue Proper
Activity 3: Supportive and Fluid Connective Tissue
Activity 4: Muscle Tissue
Activity 5: Nervous Tissue
Activity 6: Putting it All Together
Case Study: “Case of the Persistent Cough”
You are assisting a pulmonologist. The patient is a 26-year-old male who has been experiencing a painful cough for the past 6 weeks. The patient had been a chain smoker for 4 years and switched to vaping 6 months ago after hearing from friends that it was a supposedly safer alternative to smoking. An initial pulmonary CT scan showed that his lungs appeared clear. No cancerous masses or fluid accumulation were detected. The patient is referred for a bronchial biopsy.
Activity 1: Epithelial Tissue
Materials:
- compound microscope (one microscope per student)
- dropper bottle of isopropyl alcohol
- lens paper
- set of epithelial slides: simple squamous, simple cuboidal, simple columnar, ciliated pseudostratified columnar, nonkeratinized stratified squamous, and transitional
Background:
There are a total of eight types of epithelial tissue, marked by differences in shape and arrangement. The focus of the lab will be the following six tissue types: simple squamous, simple cuboidal, simple columnar, ciliated pseudostratified columnar, keratinized stratified squamous, and transitional epithelium.
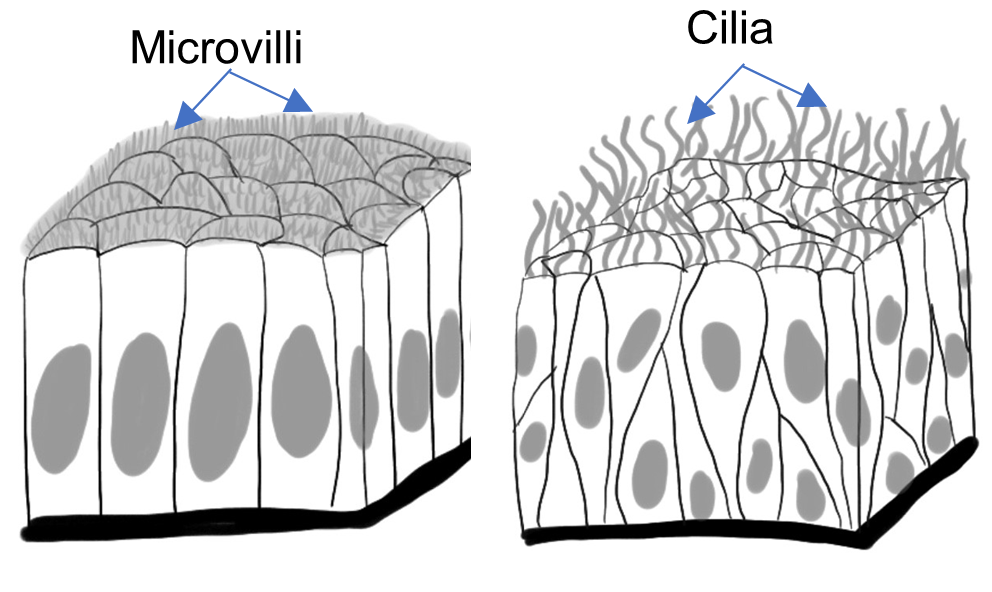
All epithelial tissue is composed of tightly packed cells. Cells are linked together by special intracellular junctions creating an effective barrier. Epithelial tissue is typically avascular, meaning that nutrients must diffuse from underlying connective tissue. Since epithelial tissue lines body surfaces, membranes, tubes, and ducts, it also exhibits polarity, meaning it has a top and a bottom. The apical surface faces the external environment or the inner surface of a body cavity (lumen). The basal surface is bound to the basement membrane and is continuous with underlying connective tissue. Often, epithelial tissue may also have cellular projections. These tiny projections may make the tissue appear fuzzy under the microscope. There are two main types of projections are cilia and microvilli. Cilia are thin, long projections that can move, while microvilli are short, dense extensions of the cell membrane for increasing surface area. Pseudostratified columnar epithelium of the trachea has cilia for moving debris out of the respiratory tract. Simple columnar epithelium of the digestive tract has microvilli for increasing absorption.
Epithelial tissue must be an effective barrier and allow for varying amounts of diffusion across its surface. Epithelial tissue can form a single layer (simple), multiple layers (stratified), or be “falsely stratified” (pseudostratified), where the cells seem to form multiple layers, but are, in fact, all part of one layer. The cells of epithelial tissue can vary in shape, from flat (squamous), to square (or as tall as they are wide) (cuboidal), to much taller than they are wide (columnar). Stratified epithelium can be tricky to identify as the cells of stratified epithelial tissue may have slightly different shapes in the deeper layers of the tissue than at the apical edge. As a rule of thumb, always look at the apical (top) layer to determine shape.
Transitional epithelium is a special type of stratified epithelial tissue found only in the urinary bladder and ureter. It has apical cells which vary in shape depending on forces applied to the tissue. The apical cells appear cuboidal when no force is applied (as when the bladder is empty) and transition to a more squamous shape when the tissue is stretched (as when the bladder is full).
Figure 1: Decision tree used to identify the types of epithelial tissue.
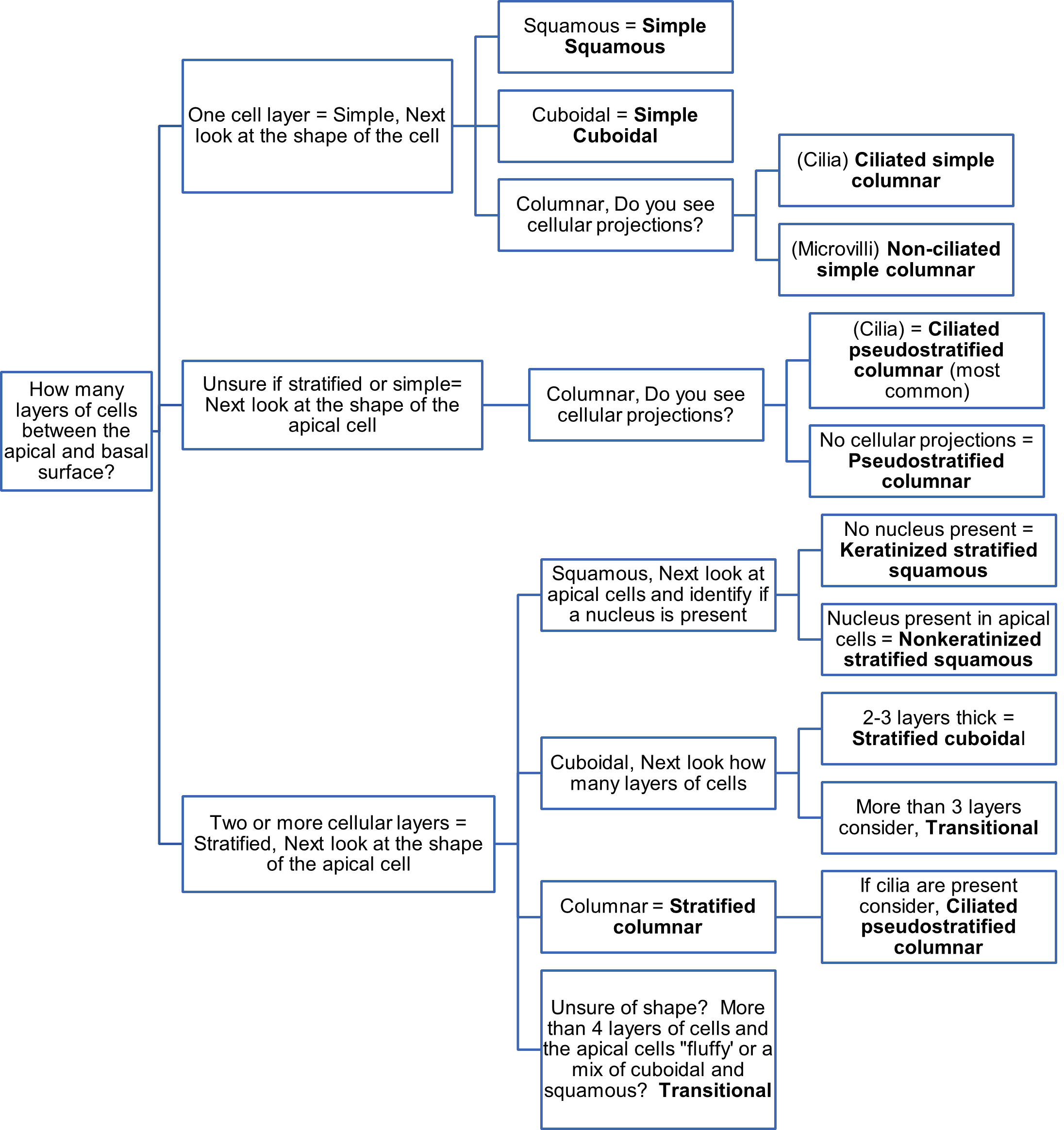
When trying to find and identify epithelial tissue on a slide it will help to use a flowchart or decision tree. Use the Figure 1 flowchart and the following questions try to identify the diverse types of epithelial tissue.
Steps to find epithelial tissue on a slide
- Look for a collection of cells that appear to line or surround a lumen or on the edge of the tissue. The cells will be in contact with the free surface creating a continuous line of cells.
- Find the cells on the apical or free surface of the tissue. Next, look for the basal surface of the tissue. Typically, you will see a darkly stained line or a change in cell type to indicate the basement membrane. Determine if all the epithelial cells are in contact with the basement membrane and if most are in contact with the apical surface. If they are, the epithelium is one cell layer thick and is called simple epithelial. If you see more than one cell layer between the apical and basement membrane, then it is stratified epithelial.
- Use Figure 1 and follow the features listed below to distinguish among the tissue types. Note that we will be identifying only six types of epithelial tissue, based on the slides available.
Tips for identifying the different epithelial tissues on a slide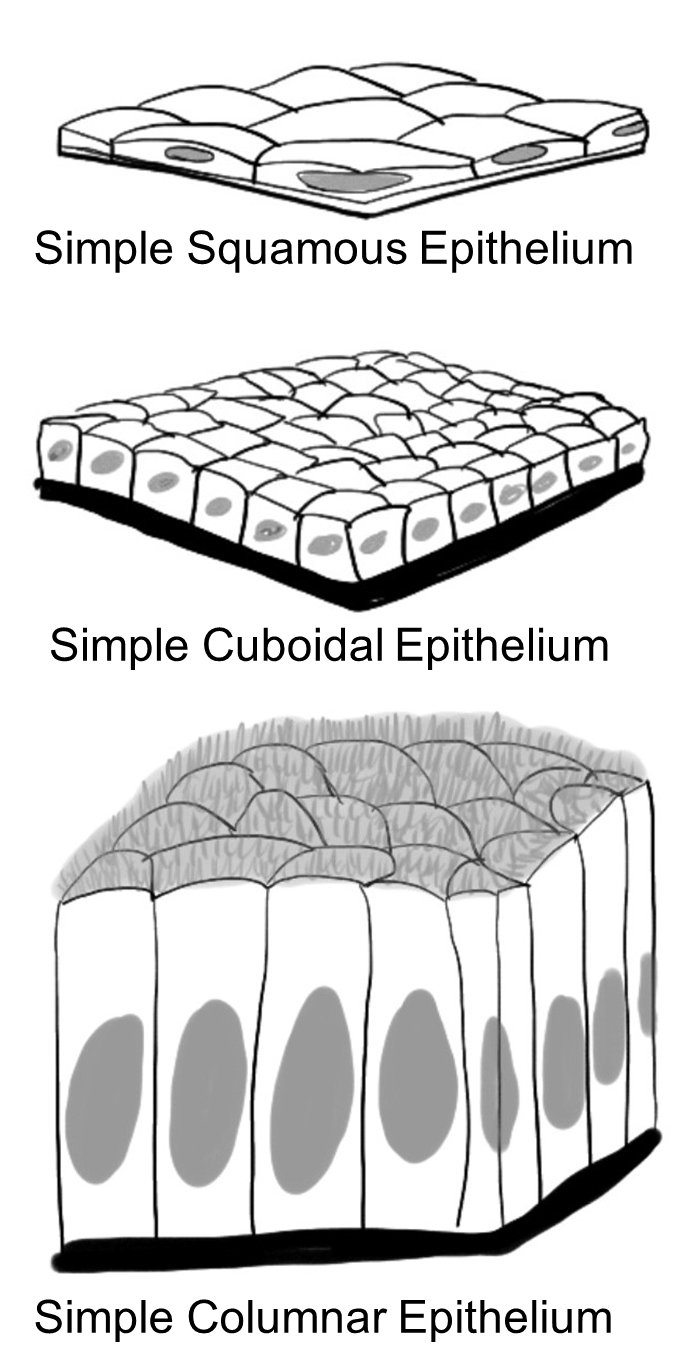
- Simple epithelial (one cell layer thick. Most cells are in contact with both the apical and basement membrane)
- Next look at the epithelial cell and determine the shape.
- Squamous (flat, or thin looking) = Simple squamous epithelium
- Cuboidal (square looking) = Simple cuboidal epithelium
- This type of epithelium may have microvilli* present
- Columnar (long, slender, or rectangular looking) with oval nuclei toward the basement membrane = Simple columnar epithelium
- Do you see surface projections from the apical membrane?
- Are the projections long and distinct? (Cilia)= Ciliated simple columnar epithelium
- Do you see a “haze” or lots of small projections packed together (brush border/ (Microvilli)? = non-ciliated simple columnar epithelium
- Are you unsure if the epithelium is stratified or simple?
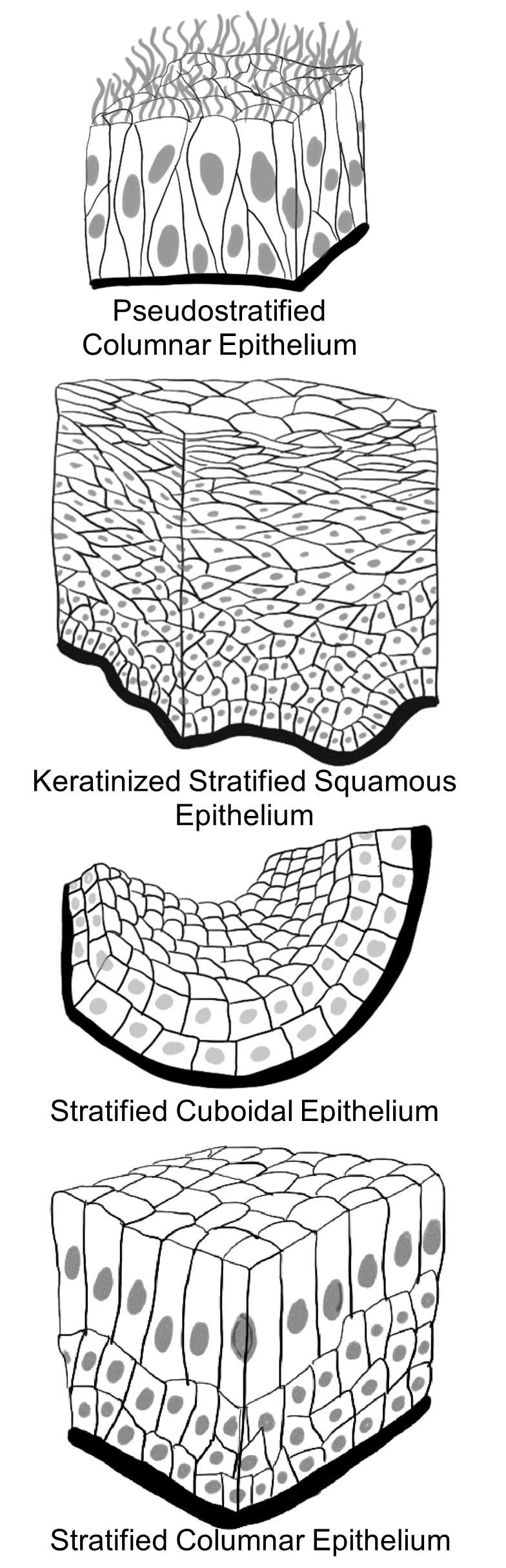
- Are most of the cells columnar, but some cells are of different heights?
- Do all the cells touch the basement membrane and not all reach the apical surface?
- Are the nuclei not in a line and look scattered? If so, you probably are observing Pseudostratified columnar epithelium.
- Stratified epithelial tissues are composed of two or more cells in between the apical and basal surface. Look at the apical epithelial cell (the cell closest to the lumen) and determine its shape.
- Squamous (flat, or thin looking).
- Look at apical cells and identify if a nucleus is present.
- No nucleus is present in apical cells, cells might look “flakey” = Keratinized stratified squamous epithelium
- Nucleus present in apical cells= Nonkeratinized stratified squamous epithelium
- Look at apical cells and identify if a nucleus is present.
- Cuboidal (square looking)
- Stratified cuboidal epithelium is typically, only two to three cells thick)
- Transitional epithelium. Transitional epithelium generally has more than four layers and appears “bubbly” on its surface.
- Columnar (long, slender, or rectangular looking)
- Do you see surface projections from the apical membrane?
- No surface projections or microvilli present = Stratified columnar epithelium
- Are the projections long and distinct? (Cilia), Consider Pseudostratified columnar epithelium.
- Squamous (flat, or thin looking).
Procedure:
1. Set up your microscope. Remember these steps!
- Plug in your microscope and turn it on.
- Make sure the scanning objective (4x, red) is in position
- If the stage is not already lowered, then use the coarse adjustment knob to lower the stage until it stops.
- Place the “sample” slide on the stage and use the stage clips to hold the slide in position.
- While watching the specimen from the side use the stage adjustment knobs, move the slide around until the specimen comes into the field of view.
- Look into the ocular lens and move the area of focus into the center of view.
- Bring the specimen into focus using the coarse adjustment knob. Once it is mostly in focus, use the fine adjustment knob to bring it into sharp focus.
- Make sure the slide is in perfect focus at scanning power (4x, red) before moving to low power (10x, yellow).
- Turn your objective without moving the slide or stage.
- Use only the fine adjustment knob to bring the specimen into sharp focus.
- Again, center the specimen before moving to the high power (40x, blue).
- At high power use only the fine focus knob and do not turn it more than 1/2 turn.
2. Using the prepared slides provided, find examples of each of the types of epithelial tissue.
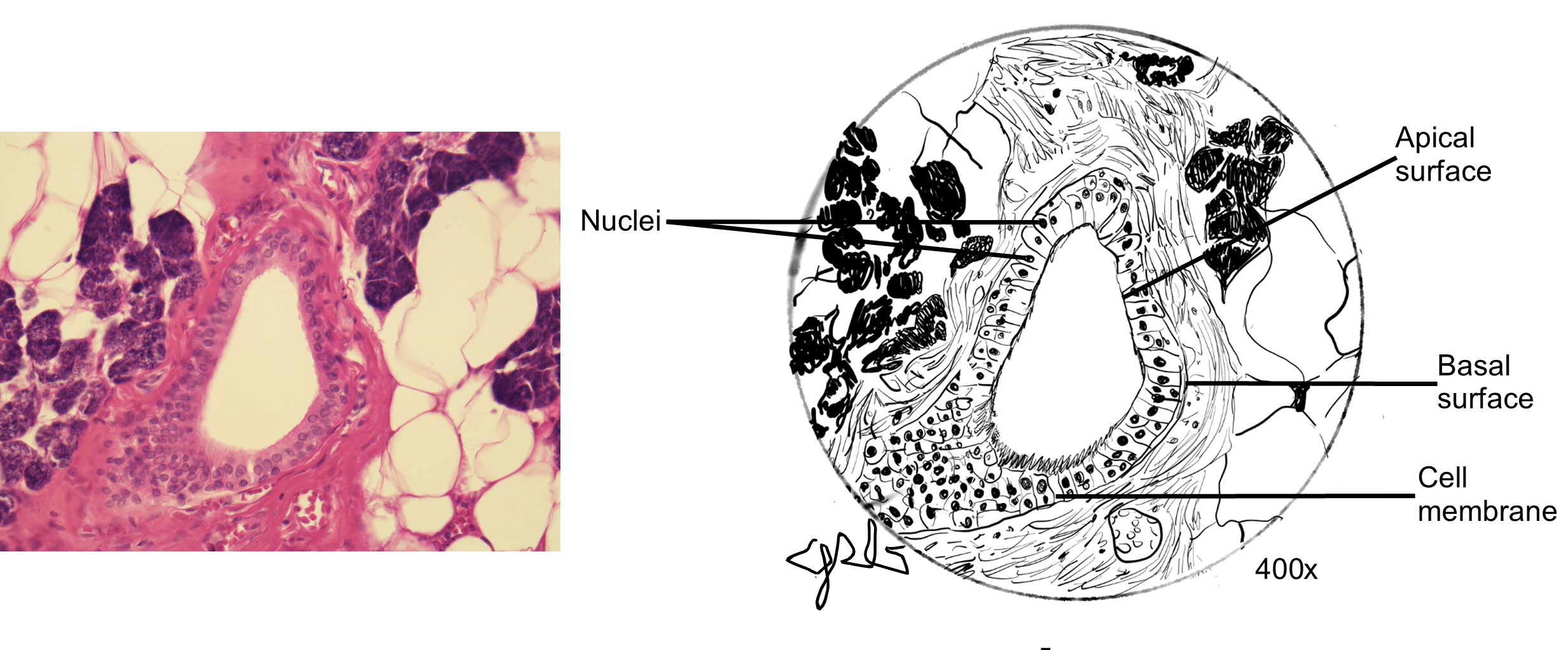
3. Observe, draw, and label the six types of epithelial tissues and label the important cellular components typical of that tissue (apical surface, basal surface, nucleus, cell membrane. And, if applicable: cilia or microvilli). Use Figure 2 as an example of how to make and label a scientific drawing.
Figure 2: Properly labeled diagrams contain straight, non-overlapping ledger lines, completely labeled with neat labels written horizontally. Drawings should be done in pencil and may be colored. The field of view should be filled.
Quick Reminders
- Layers – simple (one cell thick) or stratified (2 or more cells thick).
- Shape – Name shape epithelium by the cell layer closest to the lumen/ free surface. (apical layer)
- Squamous – squished with flat nucleus
- Cuboidal – height = width with full round nucleus
- Columnar – taller than is wide with an oval nucleus near the base
- Other non-typical descriptors – pseudostratified & transitional
- Additional characteristics to identify – keratin, cilia and microvilli
- NOTE: Since you are looking at slides from an organ or area of the body, you will often see multiple types of tissue present and even multiple types of epithelial tissue. Try to look for a pattern in the tissue and not just one or two cells. Survey the entire slide to find a section that best represents the tissue you are trying to identify.
- For more images use www.histologyguide.com to find excellent examples of the desired tissue.
Simple Squamous Epithelium
Use lung (alveolus) slide
Simple or stratified? __________________________
Cell shape: _________________________________
Are there cell membrane projections? ____________
Simple Cuboidal Epithelium
Use “cuboidal section”/kidney slide
Simple or stratified? __________________________
Cell shape: _________________________________
Are there cell membrane projections: ____________
Simple Columnar Epithelium
Use “EPITHELIUM: Columnar/intestines” slide
Simple or stratified? __________________________
Cell shape: _________________________________
Cell membrane projections: ____________
 Ciliated Pseudostratified Columnar Epithelium
Ciliated Pseudostratified Columnar Epithelium
Use “EPITHELIUM: trachea” slide
Simple or stratified? __________________________
Cell shape: _________________________________
Cell membrane projections: ____________
Simple Squamous Epithelium
Use “EPITHELIUM: small intestine” slide
Simple or stratified? __________________________
Apical cell shape: _________________________________
Keratinized or Nonkeratinized: ____________
Transitional Epithelium
Use “EPITHELIUM, urinary bladder” slide
Simple or stratified? __________________________
Apical cell shape: _________________________________
Activity 2: Connective Tissue Proper
Materials:
- compound microscope (one microscope per student)
- dropper bottle of isopropyl alcohol
- lens paper
- set of connective tissue slides: areolar, adipose, reticular, dense regular, dense irregular, and dense regular elastic
Background:
Connective tissue is the most diverse group of tissues. It can be a fluid (blood) or solid (bone). It includes tissues with high tensile strength like tendons (dense regular connective tissue), and flexible tissue like elastic cartilage or elastic tissue. Moreover, unlike epithelial tissue that consists of highly organized, tightly packed cells, connective tissue often appears disorganized and even “messy.”
Given its structural diversity, what is common to all these tissues? All connective tissue consists of cells surrounded by extracellular matrix. The most common cell is the fibroblast. Fibroblasts are responsible for producing the extracellular matrix and collagen fibers. Other cell types exist like chondrocytes in cartilage, osteocytes in bone, and the blood cells common in blood. The extracellular matrix, in turn, is made up of different fibers and a gel-like material, called “ground substance.” The most common fibers are collagen, elastic, and reticular. All of these protein fibers give the connective tissue its tensile strength. However, each type of fiber has different properties that contribute to the different connective tissue functions. Collagen is the most common fiber and can be described as long cables. Collagen fibers are flexible and provide a lot of tensile strength. Elastic fibers typically appear wavy and have the ability of being able to stretch and recoil. Reticular fibers are short and branched. Reticular fibers form a mesh to anchor and support the embedded cells.
Different ground substances allow some connective tissue to be fluid like blood, gel-like like cartilage, or hard, like bone. Here you will investigate eleven of the thirteen different types of connective tissue. Each has its own unique combination of cells and extracellular matrix, and its own combination of fiber and ground substance types.
Connective tissue = Cells + Extracellular matrix (Fibers + Ground substance)
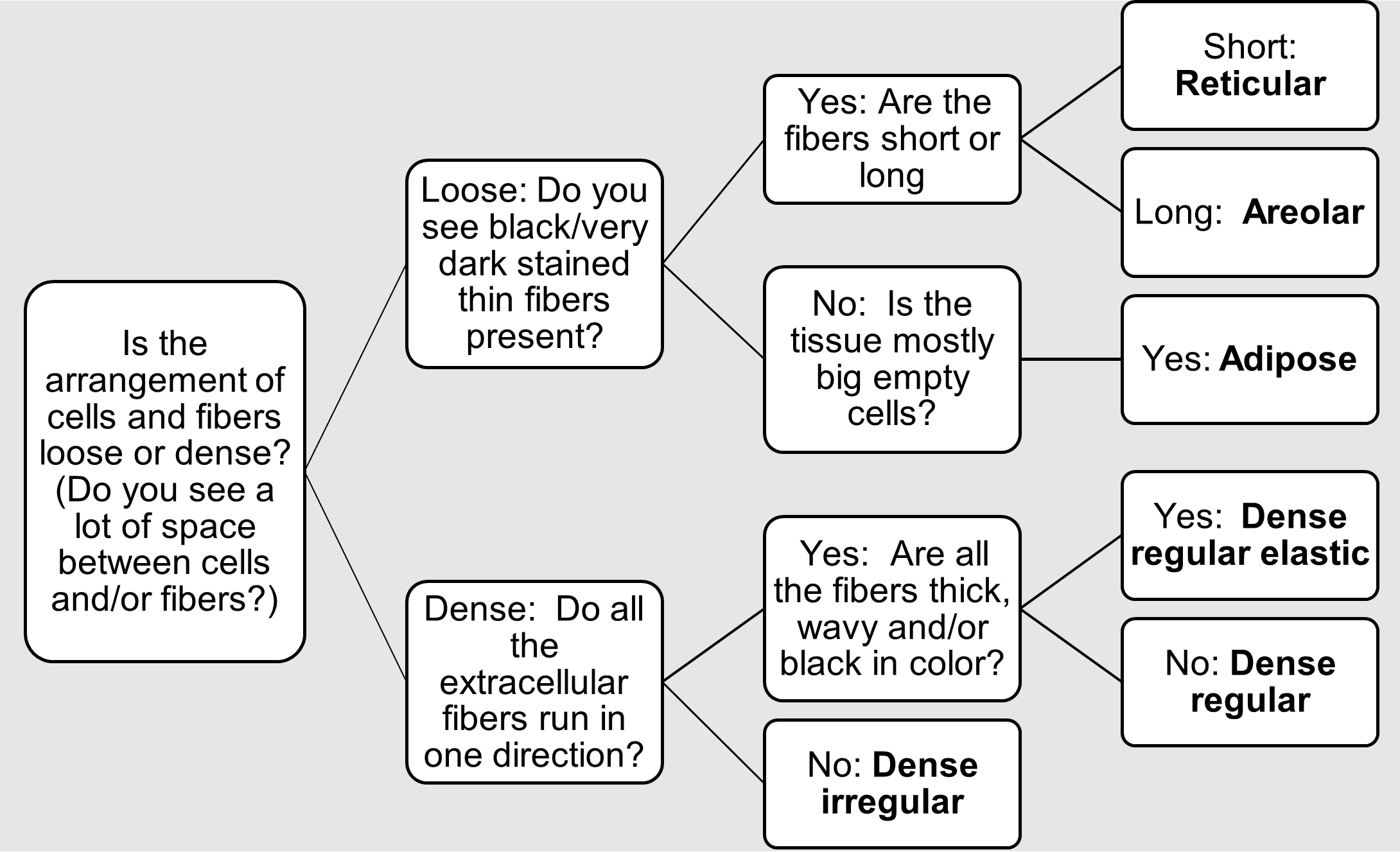
Connective tissue proper can be sub-divided into loose and dense connective tissue. The ground substance is viscous (gel-like) in both types, but the arrangement of fibers is different. Loose connective tissue features fibers that spread out, often extending in many different directions. The ground substance is easily visible. Examples include areolar tissue, adipose tissue, and reticular tissue. Dense connective tissue features a high density of fibers with little visible ground substance. This creates a tissue that is stronger, and includes examples such as dense regular tissue, dense irregular tissue, and elastic connective tissue.
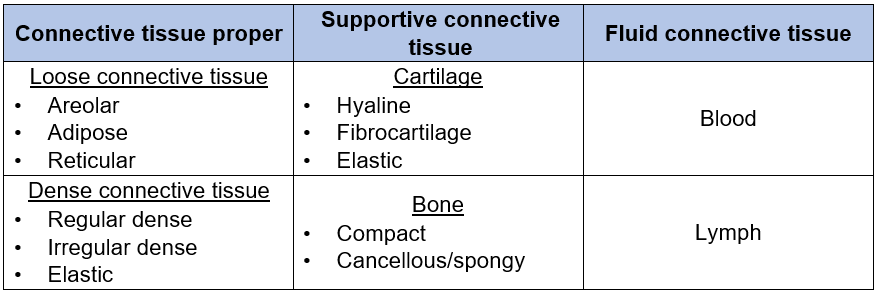
We will discuss the supportive connective tissue (compact bone and the three types of cartilage) and fluid connective tissue (blood) in the next activity.
Table 2: The main categories of connective tissue and the 13 subtypes of connective tissue.
Hints to identify connective tissue proper on a slide
- First determine that you are observing connective tissue, not epithelial tissue. Cells of connective tissue are not tightly packed like epithelial tissue; cells will appear scattered. Connective tissue will lack a free edge, as it lies under other tissues.
- Determine if you have fluid, supportive, loose, or dense connective tissue type (you may need to use a reference book for images). To distinguish among the loose and dense connective tissue subtypes, pay close attention to the density of the fibers and the appearance of the cells. Use the decision tree (Figure 3) to help you.
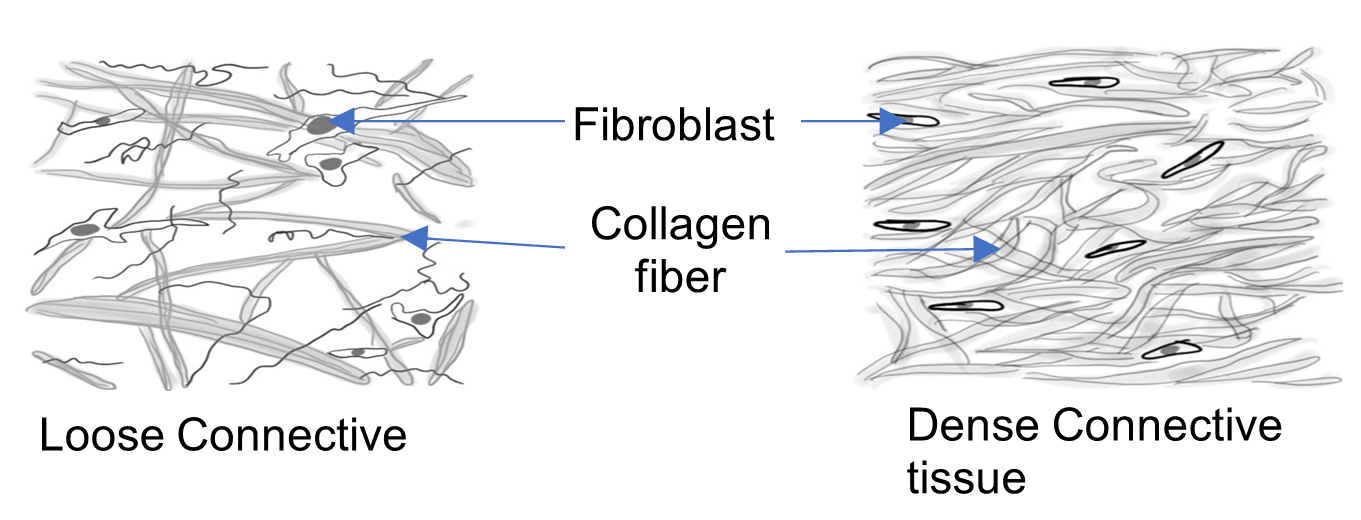
- Look at the fibers present and determine the fiber type (elastic, collagen, and/or reticular).
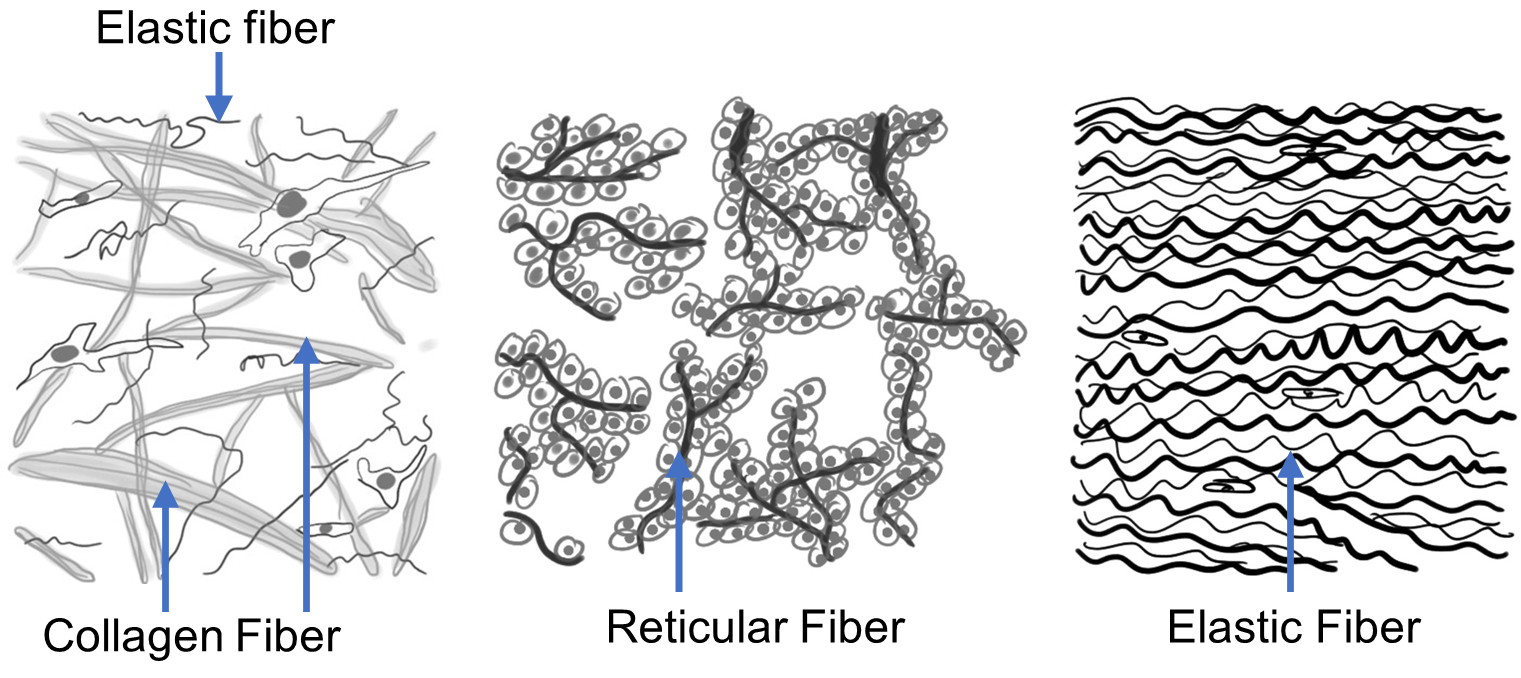
Figure 3: Decision tree used to identify loose and dense connective tissue subtypes.
Procedure:
- Observe, draw, and label the six examples of connective tissue proper and label the important cell and fiber types typical of that tissue. Some examples include: type of cell (ex: fibroblast), fiber type (elastic, collagen, and/or reticular), and ground substance. Use Figure 2 as an example of how to make and label a scientific drawing.
Areolar tissue
Use “CONNECTIVE: areolar” slide
Circle the density of fibers: dense or loose
Circle all fiber types of present:
elastic, reticular, and/or collagen
Circle the organization to fibers:
arranged in parallel or randomly scattered
Adipose tissue
Use “CONNECTIVE: adipose” slide
Adipose has collagen fibers but they are difficult to see.
What cell type is visible: _________________________
Reticular tissue
Use “CONNECTIVE: reticular tissue” slide
Circle the density of fibers: dense or loose
Circle all fiber types of present:
elastic, reticular, and/or collagen
Circle the organization to fibers:
arranged in parallel or randomly scattered
Dense regular collagenous
Use “CONNECTIVE: tendon-muscle junction” slide
Circle the density of fibers: dense or loose
Circle all fiber types of present:
elastic, reticular, and/or collagen
Circle the organization to fibers:
arranged in parallel or randomly scattered
Dense irregular collagenous
Use “CONNECTIVE: skin” slide (can also observe on trachea slide)
Circle the density of fibers: dense or loose
Circle all fiber types of present:
elastic, reticular, and/or collagen
Circle the organization to fibers:
arranged in parallel or randomly scattered
Dense regular elastic tissue
Use “CONNECTIVE: aorta” slide
Circle the density of fibers: dense or loose
Circle all fiber types of present:
elastic, reticular, and/or collagen
Circle the organization to fibers:
arranged in parallel or randomly scattered
Activity 3: Supportive Connective tissue
Materials:
- compound microscope (one microscope per student)
- dropper bottle of isopropyl alcohol
- lens paper
- prepared slides of elastic cartilage, hyaline cartilage, fibrocartilage, compact bone and blood.
Background:
In this activity, we investigate the cells, fibers, and ground substance typical of supportive and fluid connective tissue. Supportive connective tissue consists of compact bone, spongy bone and three types of cartilage (hyaline cartilage, elastic cartilage, and fibrocartilage). We will investigate all of these except spongy bone in this activity.
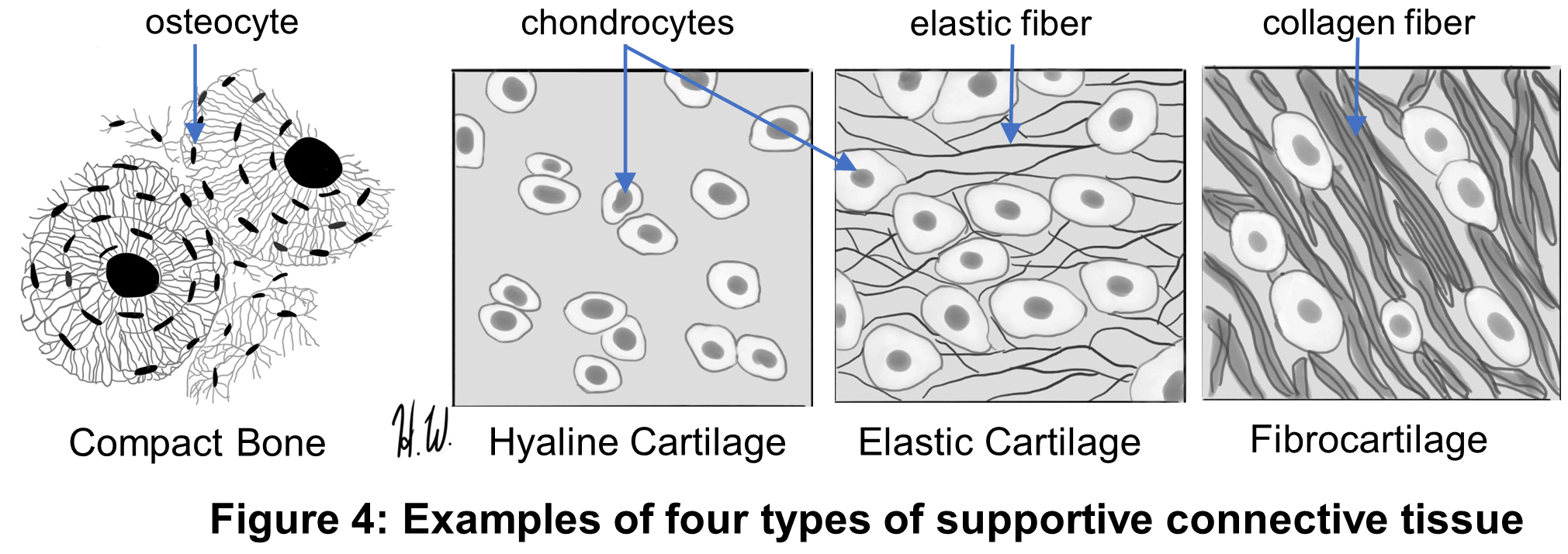
Bone connective tissue has cells called osteocytes. They live within cavities called lacunae. The cells of cartilage are called chondrocytes. They, too, live within lacunae. Collagen is the most common fiber type found in compact bone, spongy bone and fibrocartilage; elastic fibers are embedded in elastic cartilage. The ground substance of the supportive tissues sets these tissues apart from other connective tissues.
Bone and cartilage each have a unique matrix, made of different ground substances. Compact bone contains a hardened calcified matrix. The ground substance is rigid due to the inorganic calcium salts deposited amongst the collagen fibers. Another unique characteristic of compact bone is its arrangement in concentric rings called osteons. All three cartilage types (hyaline cartilage, elastic cartilage and fibrocartilage) have a gel like, squishy ground substance made of glycosaminoglycans such as hyaluronic acid and chondroitin sulfate. This slippery, putty-like ground substance makes cartilage flexible and a good cushion. The fiber content varies from few collagen fibers (hyaline cartilage) to many collagen fibers (fibrocartilage) or perhaps elastic fibers instead (elastic cartilage).
Figure 4: Examples of four types of supportive connective tissue
Fluid connective tissue, blood, has a ground substance composed mainly of water, called plasma. The watery plasma contains dissolved proteins and electrolytes. The blood cells (red blood cells, white blood cells, and platelets) are suspended in the plasma. There are no fibers to speak of in normal blood. Red blood cells are anucleate (no nucleus), white blood cells have uniquely shaped nucleus, and platelets are small, cell fragments.
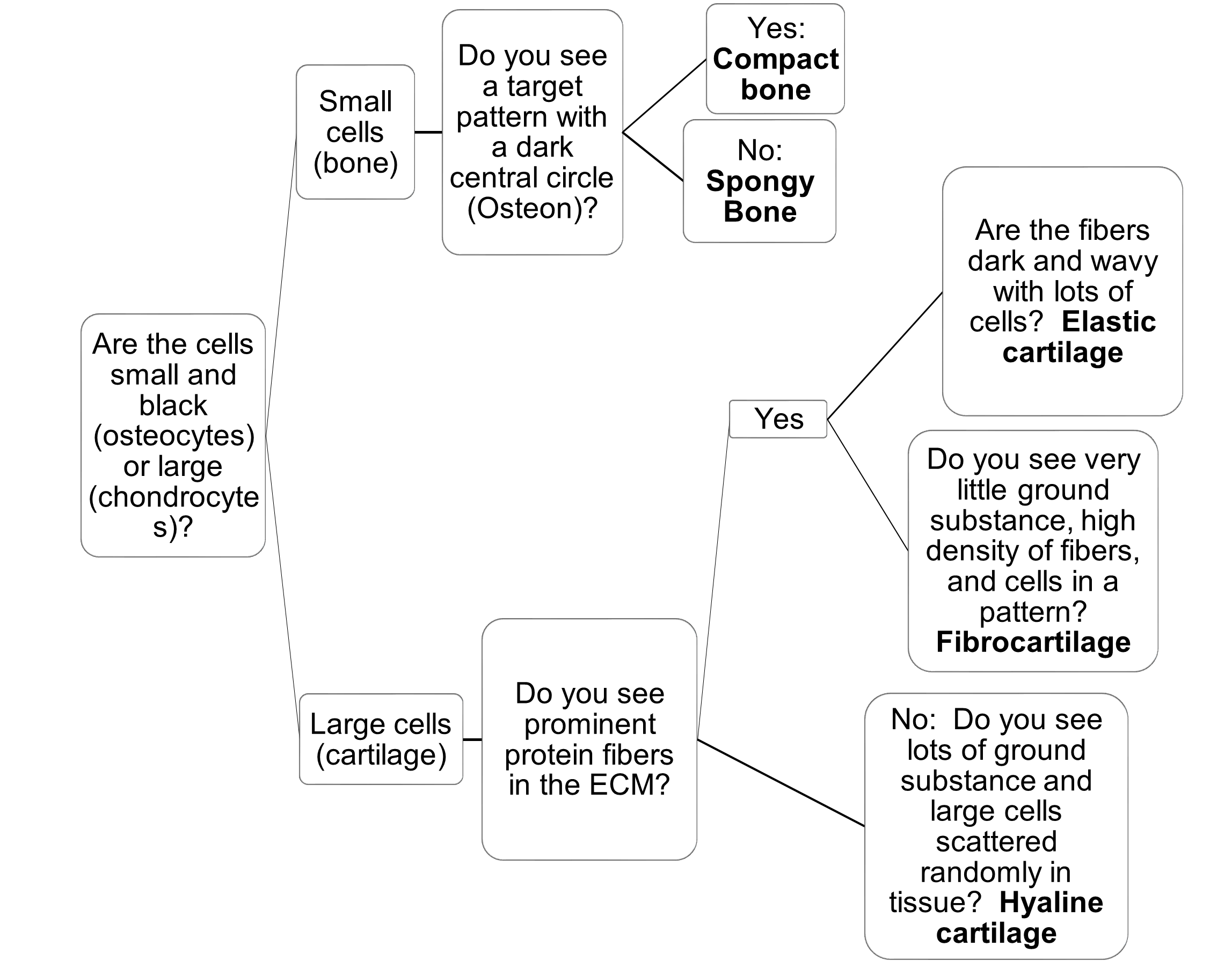
Hints to identify supportive connective tissue types.
Cartilage: Look closely at the size of the cells. If the cells have prominent nuclei and are larger you have cartilage. To determine which of the three types of cartilage it is, determine the differences in the density and appearance of their fibers (Figure 4). Cartilage without prominent fibers visible is hyaline cartilage. Prominent collagen fibers are embedded in fibrocartilage, and prominent embedded elastic fibers make up elastic cartilage.
Compact Bone: If the cells are small, it is likely compact bone. Compact bone has the distinctive characteristic that the cells are arranged in concentric rings, a structure called an osteon (Figure 4). Use the decision tree to distinguish among the supportive connective tissue types (Figure 5).
Figure 5: Decision tree used to identify supportive and fluid connective tissue types.
Procedure:
- Set up your microscope.
- Using the prepared slides provided, find examples of each of the four types of supportive tissue and one type of fluid connective tissue. We will not observe spongy bone.
- Use scanning power (4x, red), and then low power (100x, yellow) to find each image. Then use high power (40x, blue) to properly draw and label each connective tissue type. Use the terminology sheet and a textbook to help you thoroughly label each tissue type. Some examples of appropriate labels include: type of cell (ex: chondrocyte, osteocyte, red blood cell, or white blood cell), fiber type (elastic, collagen, and/or reticular), ground substance (calcified, gel-like, or watery)
Hyaline cartilage
Cell type(s) common: ____________________________
Type of fiber present (if any): ______________________
Elastic cartilage
Cell type(s) common: ____________________________
Type of fiber present (if any): ______________________
Fibrocartilage
Cell type(s) common: ____________________________
Type of fiber present (if any): ______________________
Compact bone
Cell type(s) common: ____________________________
Type of fiber present (if any): ______________________
Blood
Are fibers present? _____________
What is the ground substance of this tissue called? _____________
Name three specific cell types you observe:
1) __________________
2) __________________
3) __________________
Activity 4: Muscle Tissue
Materials:
- none
Background:
Muscle tissue is a collection of cells that can contract (shorten), and thus generate a force. The cells in muscle tissue are excitable and require a stimulus. Muscle tissue can be characterized based on the presence of striations, cell shape, number of nuclei, location in body, and innervation type. The three types of muscle tissue are skeletal, cardiac, and smooth (Figure 6). Muscle tissue contains protein fibers which help the cells contract. When the protein fibers are densely packed and arranged in an organized fashion, striations, or a striped appearance, this type of tissue is defined as striated muscle tissue. Both skeletal and cardiac muscle have striations. Smooth muscle tissue has protein fibers, but they are dispersed through the cell and are not clearly visible. Cardiac muscle has a distinct branching pattern and darkly stained bodies called intercalated disks at the cell junctions.
Figure 6: Representative drawings of the three types of muscle tissue, skeletal, cardiac, and smooth.
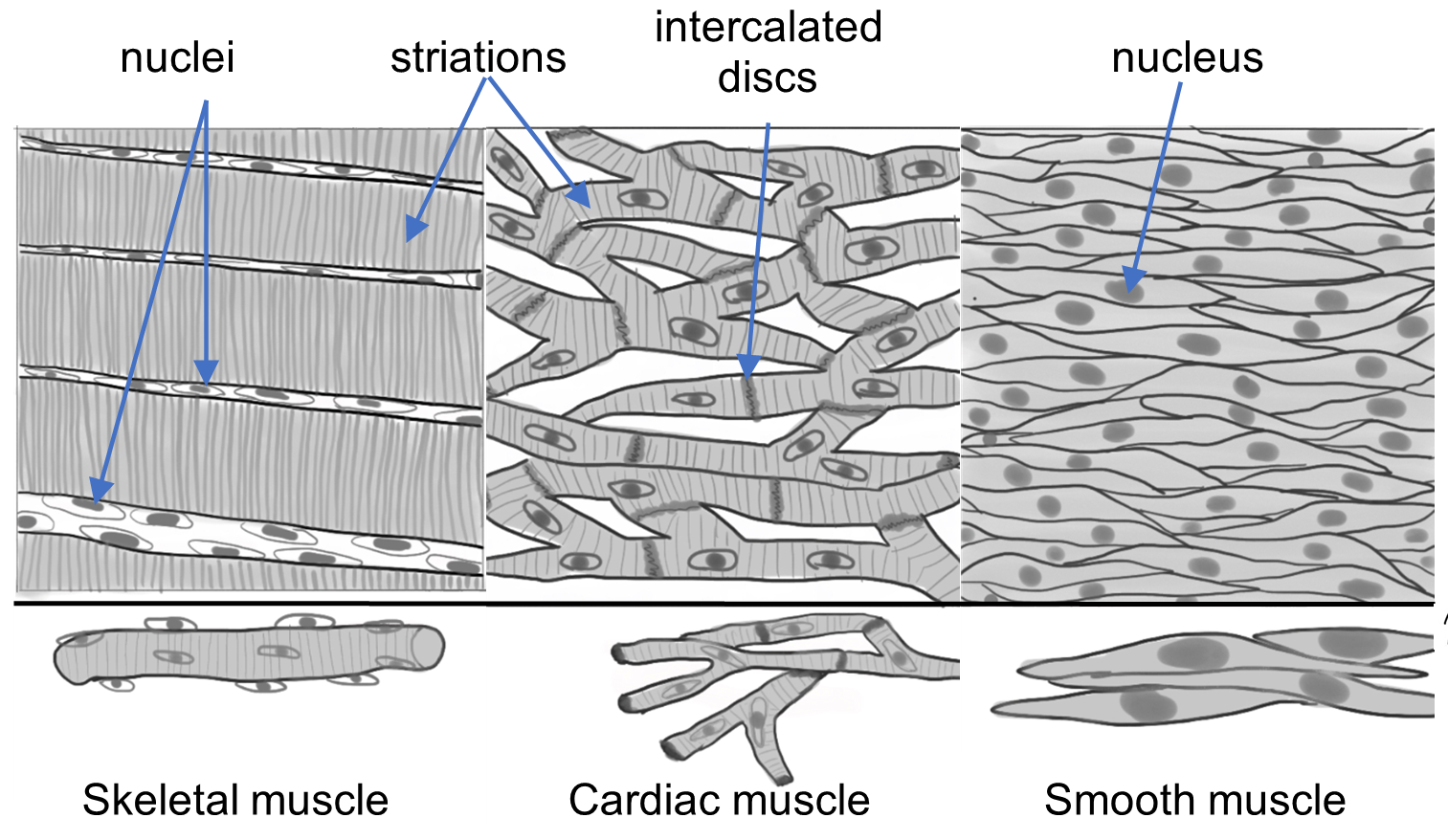
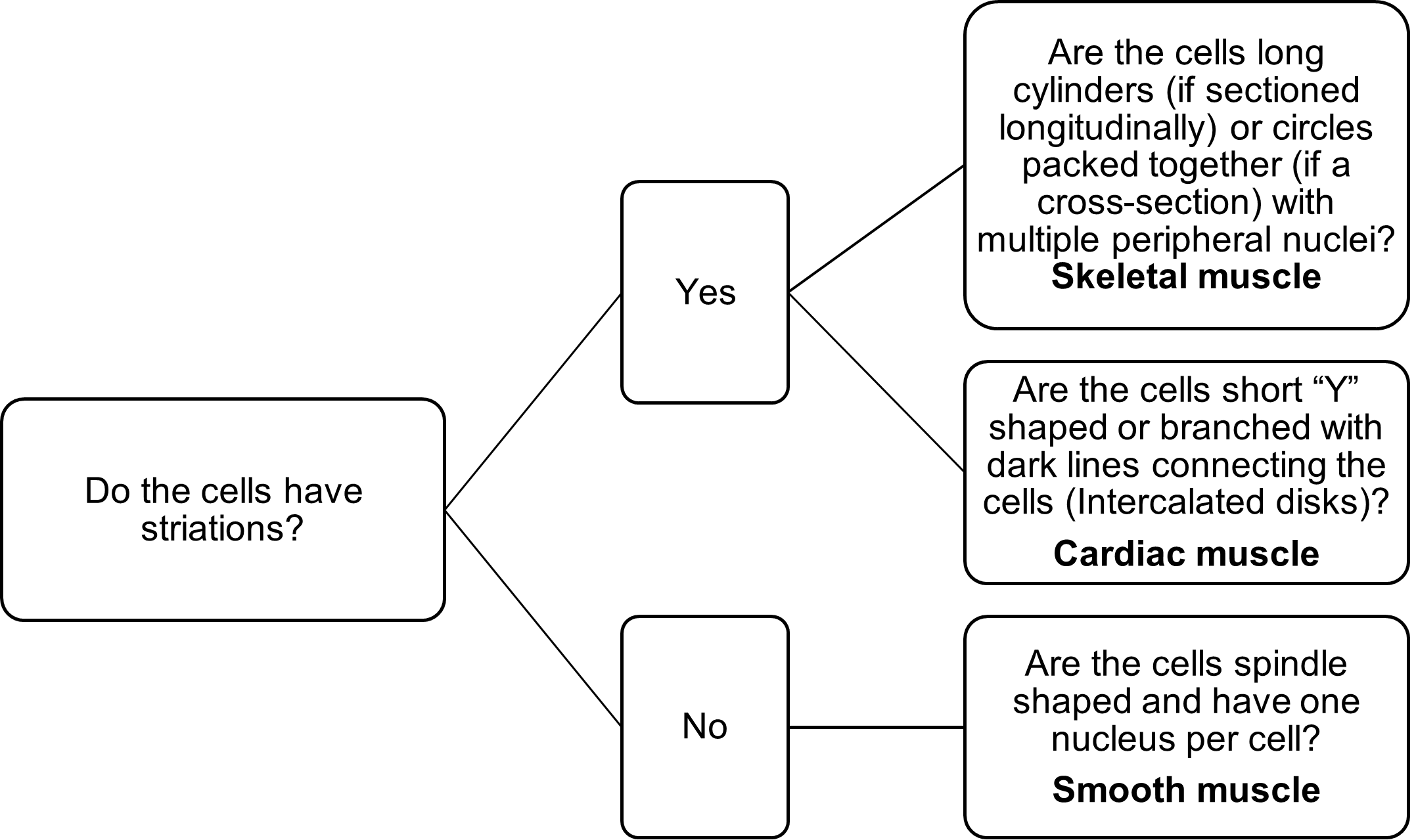
Hints to identify muscle tissue:
- Smooth Muscle: Look closely for the presence of striations (striped appearance). If the tissue lacks striations, it is smooth muscle.
- Skeletal Muscle: If the tissue is striated and has long parallel cells, it is skeletal muscle.
- Cardiac Muscle: If it has striations and short, branched cells and darkly stained borders between cells (called intercalated disks), it is cardiac muscle tissue.
- Use the decision tree to help you distinguish among these tissue types (Figure 7).
Figure 7: Decision tree used to identify among the three types of muscle tissue.
Procedure:
1. On each of the images provided below, please label the following: nucleus, muscle fiber, striation (if applicable) and intercalated disk (if applicable). Use your textbook or histologyguide.com as a resource to ensure you are looking at the right type of tissue.
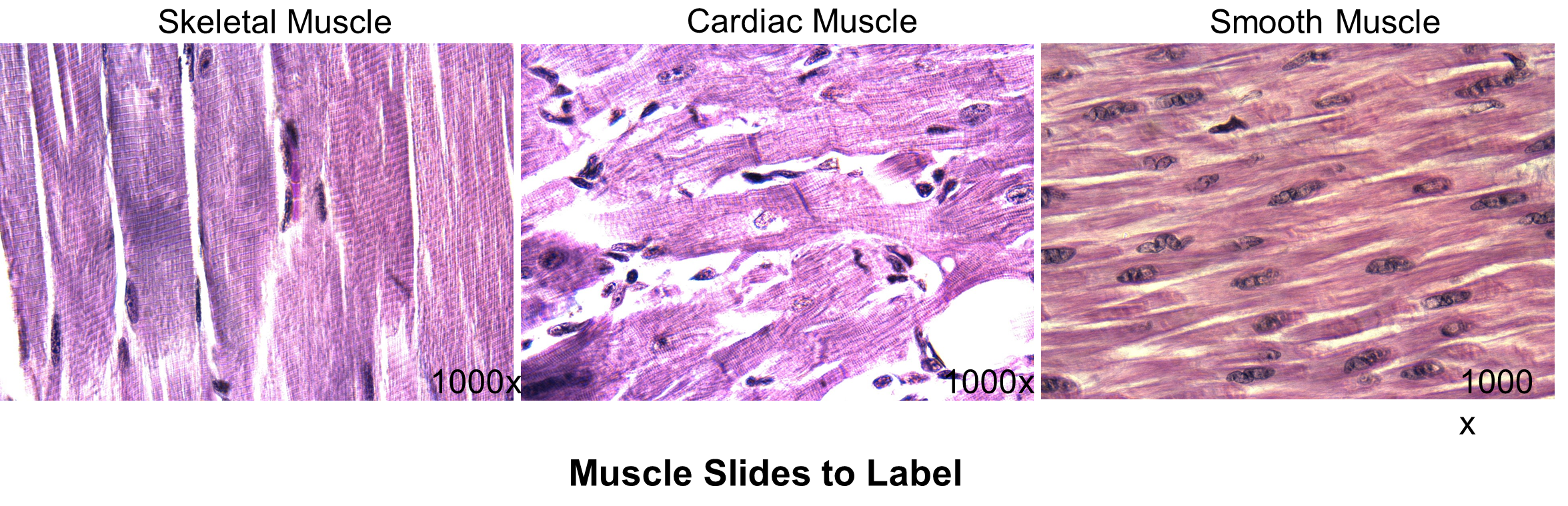
2. Look at the slide labeled “muscle tissue”. Identify each of the three types of muscle tissue on the slide. Put your pointer on smooth muscle under 400x. Show your instructor.
Smooth Muscle: Instructor’s initials: ______
3. Complete the table below using the background information and images.
| Skeletal Muscle | Cardiac Muscle | Smooth Muscle | |
| Are striations present? | |||
| Number of nuclei | |||
| Cell shape |
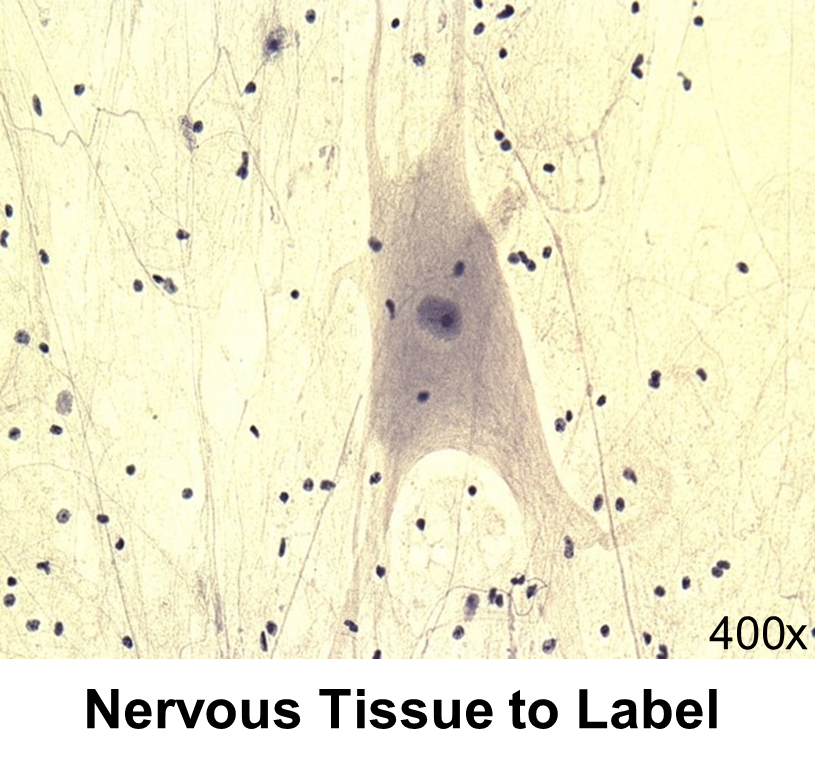
Activity 5: Nervous Tissue
Materials:
- none
Background:
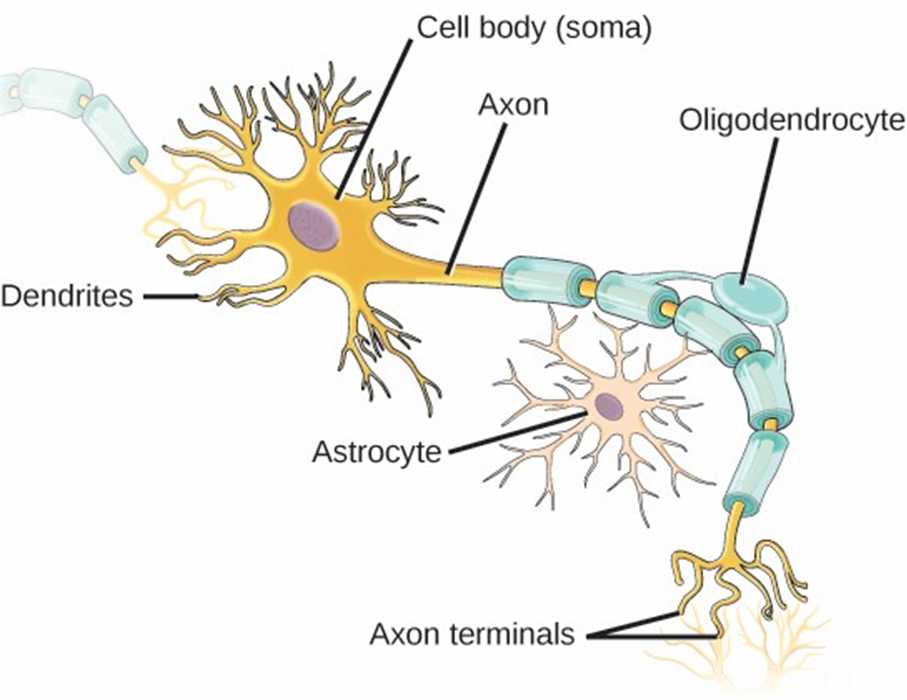
Nervous tissue is made up of two cell types: neurons and neuroglia. Neurons are excitable cells that can receive and transmit signals. They typically have a long extension, an axon, which transmits electrical signals much like an electric wire. The axon is attached to a spherical cell body that houses the nucleus and other cellular components. Dendrites also extend from the cell body and function much like antennae as they receive chemical signals from other cells. (Figure 8)
Neuroglial cells do not transmit electrical signals and instead nourish and protect the neurons. Neuroglial cells are much smaller and typically more numerous than neurons.
Figure 8: Drawing of a neuron (nerve cell).
Procedure:
1. Using the image provided, label the neuron surrounded by its neuroglial cells. On the image to the right, please label the following: cell body, nucleus, cellular extensions (axons or dendrites), neuroglial cells.
Activity 6: Putting it All Together
Materials:
- compound microscope (one microscope per student)
- dropper bottle of isopropyl alcohol
- lens paper
- microscope slide of a cross-section from an unlabeled organ
Background:
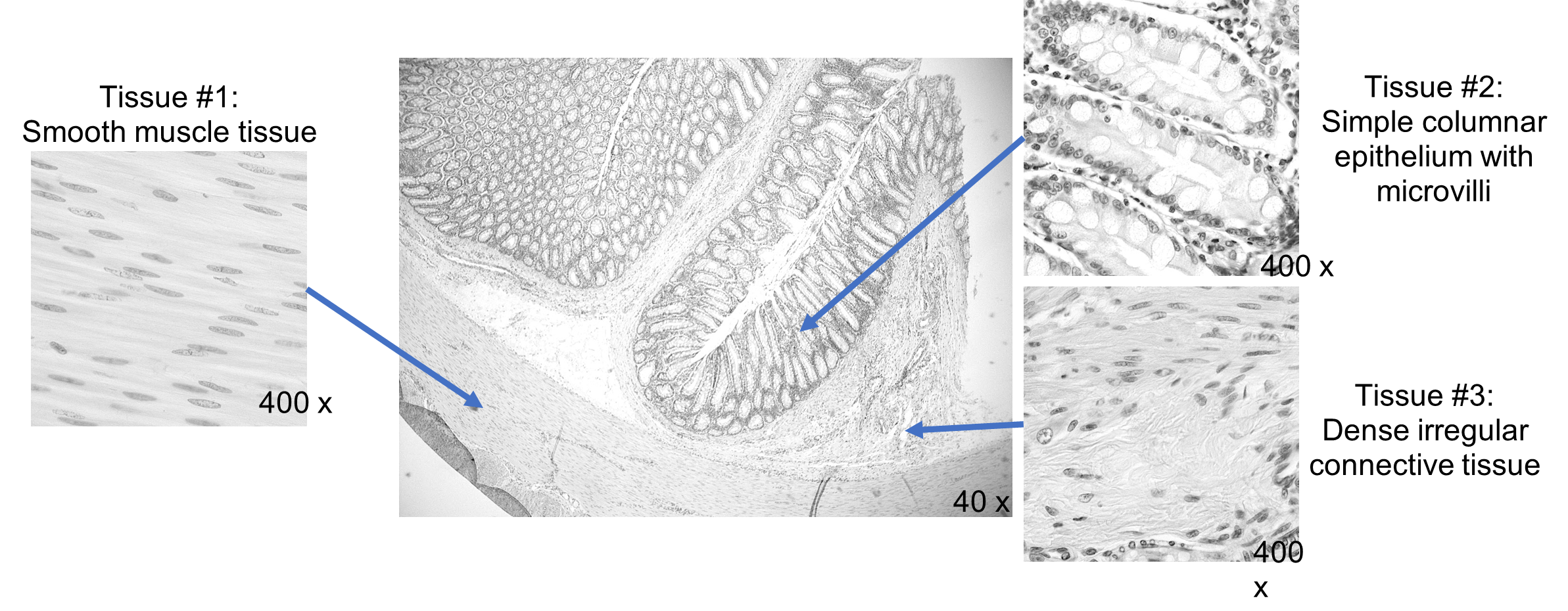
An organ is composed of two or more tissue types. Most organs in the body have all four tissues present. Now that you have identified the different tissues individually and are familiar with their primary location and general functions, let’s look at an organ to investigate how the various tissues contribute to the function of an organ (Figure 9).
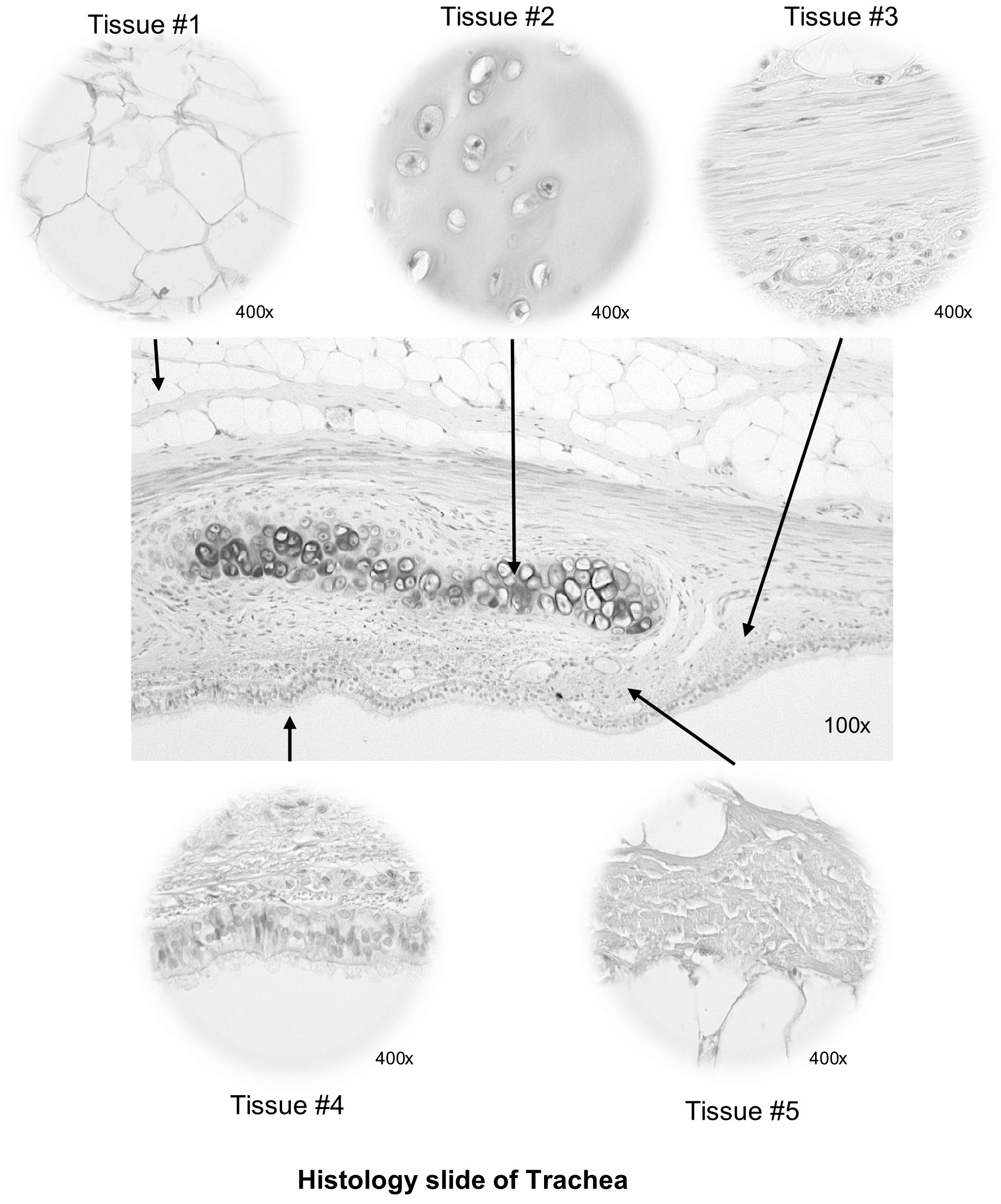
Our patient went for a bronchial biopsy to look for abnormalities in the tissue layers of the bronchus which might be leading to their symptoms. As the trachea is an organ, it is composed of all four of the types of tissue (epithelial, connective, muscular, and nervous).
Before you analyze the tracheal tissues under the microscope, let’s practice the skills needed using the intestine. The intestine is a muscular tube that absorbs a lot of water, as well as nutrients, vitamins, and minerals. Observe Figure 9 and identify the following tissues that make up this organ. It is lined with simple columnar epithelium, cells that are well-structured for absorption and for protection. Connective tissue serves to connect the epithelium with underlying tissues. Dense irregular connective tissue is flexible yet sturdy enough to play this role. The intestine undergoes waves of involuntary muscle contraction called peristalsis to propel the digested food along its length. Smooth muscle tissue is best suited for this job. These three tissue types are visible in a single slide of a cross-section of small intestine (Figure 9). Bundles of nerve fibers may also be visible in some sections, as well as blood vessels containing blood tissue.
Figure 9: Cross section of the intestine with 3 insets showing the three different types of tissue that compose the wall of the intestines.
Procedure:
1. Below is an image of the trachea from your patient’s bronchial biopsy. Under each image, label the different tissue types visible in the trachea.
2. In your integument slide box, find a slide labeled “Activity 6, #2”. This is an unknown. Look at this tissue under the microscope and identify an example of each of the three tissue types (listed below). List which specific type of tissue you identified. Before you put the slide away, have your instructor verify one of the tissue types you identified.
-
- Epithelial Tissue: __________________________________
- Connective Tissue: ________________________________
- Muscle Tissue: ___________________________________
Instructor’s initials for proper tissue identification: ______
3. Follow the steps below to properly put your microscope away.
- Turn off the power to the microscope, unplug it, and carefully fold cord and place it in the microscope pocket.
- Lower the microscope stage to its lowest position (away from the objective lenses)
- Remove any slide on the stage and rotate the nosepiece to the scanning objective.
- Use lens paper and lens-cleaning fluid to carefully clean the objectives and the ocular lenses.
- Return the microscope to its proper storage location, making sure to carry the microscope properly with both hands—holding the handles of the microscope.
- Place microscope in the cabinet with the oculars facing out and the front of the microscope in.
Creative Commons Citations:
- Histology Lab, Case-Study Based OER Lab Manual for A&P I © 2022 by G. Backus, H. Wangerin, P. Rodgers is licensed under CC BY-NC-SA 4.0.
- Figure 8. © 2022 OpenStax Anatomy and Physiology 2e licensed under CC BY 4.0
- Figures 1, 3, 4, 5, 6, 7, and 9: © 2022 by H. Wangerin is licensed under CC BY-NC-SA 4.0
- Simple Squamous Epithelium, Simple Cuboidal Epithelium, Simple Columnar Epithelium, Microvilli, Cilia, Pseudostratified Columnar Epithelium, Keratinized Stratified Squamous Epithelium, Stratified Cuboidal Epithelium, Stratified Columnar Epithelium, Loose Connective, Dense Connective, Collagen Fiber, Reticular Fiber, Elastic Fiber, Muscle Slides to Label, Nervous Tissue to Label Histology Slide of Trachea, and Panel Slides of Esophagus: © 2022 by H. Wangerin is licensed under CC BY-NC-SA 4.0.
- Figure 2 © 2022 by G. Backus is licensed under CC BY-NC-SA 4.0.

